
Annex 4
NCP: Laboratory Testing Guideline
This technical guideline is formulated to guide disease control agencies and relevant institutions at all
levels to carry out laboratory testing for NCP.
I. Specimen Collection
1. Target of collection
Suspected cases and clustered cases and others requiring diagnosis or differential diagnosis for novel
coronavirus infection; or other environmental or biological substances that require further screening
and testing.
2. Collection requirements
1) The novel coronavirus testing specimens shall be collected by qualified technicians who have
received biosafety training (who have passed the training) and are equipped with the corresponding
experimental skills. Personal protective equipment (PPE) requirements for sampling personnel are:
N95 masks or masks with higher filtration efficiency, goggles, protective clothing, double-layer latex
gloves and waterproof boot covers; the outer layer of the latex gloves shall be changed in a timely
manner should sampling personnel touch patients’ blood, body fluids, secretions etc.
2) Specimens of inpatient cases shall be collected by medical staff of the hospital where they are being
treated.
3) Specimens of close contacts shall be collected by the designated local CDCs and medical institutions.
4) Multiple specimens may be collected in the course of the disease, depending on the need of
laboratory testing.
3. Categories of specimens collected
Respiratory tract specimens in the acute phase (including upper or lower respiratory tract
specimens) must be collected from each case; lower respiratory tract specimens shall be preferred
for the collection from severe cases. Stool samples, whole blood samples and serum samples can be
collected according to clinical needs.
Categories of specimen:
1) Upper respiratory tract specimens: including nasopharyngeal swabs, pharyngeal swabs etc.
2) Lower respiratory tract specimens: including deep-cough sputum, alveolar lavage fluids, bronchial
lavage fluid and respiratory tract extracts.
3) Fecal specimens: Fecal samples are about 10 g (peanut size). If it is not convenient to collect fecal
samples, an anal swab can be collected.
4) Blood specimens: One should, as much as possible, collect anticoagulated blood in the acute phase
within 7 days after the onset of disease. 5 ml of blood is required for each collection. Vacuum tubes
containing EDTA anticoagulant are recommended in blood collection.
5) Serum specimens: Both acute-phase and convalescent serum specimens should be collected as
much as possible. The first serum specimen should be collected as soon as possible (preferably within
7 days after the onset of illness), and the second specimen should be collected during 3-4 weeks after
the onset of illness. 5 ml of blood is required for each specimen and vacuum tubes without
anticoagulant are recommended. Serum specimens are mainly used for measuring antibodies, rather
than nucleic acid testing.
4. Methods of specimen collection and processing
1) Nasopharyngeal swab: The sampler gently holds the person's head with one hand, the swab in
another, insert the swab via nostril to enter, slowly get deep along the bottom of the lower nasal canal.
Because the nasal canal is curved, do not force too hard to avoid traumatic bleeding. When the tip of
the swab reaches the posterior wall of the nasopharyngeal cavity, rotate gently once (pause for a
moment in case of reflex cough), then slowly remove the swab and dip the swab tip into a tube
containing 2-3ml virus preservation solution (or isotonic saline solution, tissue culture solution or
phosphate buffer), discard the tail and tighten the cap.
2) Pharynx swab: the sampled person first gargles with normal saline, the sampler immerses the swabs
in sterile saline (virus preservation solution is not allowed to avoid antibiotic allergies), holds the head
of the sampled person up slightly, with one’s mouth wide open, making a sound "ah" to expose the
lateral pharyngeal tonsils, insert the swabs, stick across the tongue roots, and wipe both sides of the
pharyngeal tonsils with pressure at least 3 times, then wipe on the upper and lower walls of the
pharynxat for at least 3 times, and dip the swabs in a tube containing 2-3ml storage solution (or
isotonic saline solution solution, tissue culture solution or phosphate buffer solution), ), discard the
tail and tighten the cap. The pharyngeal swabs can also be placed in the same tube together with the
nasopharyngeal swab.
3) Nasopharyngeal or respiratory tract extract: Extract mucus from the nasopharynx or extract
respiratory secretions from the trachea with a collector connected to a negative-pressure pump; insert
the head of the collector into the nasal cavity or trachea, turn on the negative pressure, rotate and
slowly withdraw the head of the collector, collect the extracted mucus, and rinse the collector once
with 3 ml of sampling solution (a pediatric catheter connected to a 50-ml syringe may be used as an
alternative to the collector).
4) Deep cough sputum: Ask the patient to cough deeply, and collect the sputum coughed up in a 50-
ml screw-capped plastic tube containing 3 ml of sampling solution. If the sputum is not collected in
the sampling solution, 2-3 ml of the sampling solution can be added into the tube before testing, or
add sputum digestive reagents of equal volume of sputum.
Formula of storage fluid for sputum digestive reagents:
Ingredients
Per Bottle
Dithiothreitol
0. 1g
Sodium chloride
0.78g
Phosphorus chloride
0.02g
Disodium hydrogen phosphate
0.112g
Potassium dihydrogen phosphate
0.02g
Water
7.5ml
pH 7.4
±
0.2(25
°
C)
Dilute the storage solution to 100 ml with deionized water before use. Sputum can also be treated
with a phosphate buffer containing 1 g/L of protease K in an equal volume of sputum.

5) Bronchial lavage fluid: Insert the head of the collector into the trachea (about 30cm deep) from
the nostril or the tracheal insertion part, inject 5 ml of physiological saline, turn on the negative
pressure, rotate the head of the collector and slowly withdraw it. Collect the extracted mucus and
rinse the collector once with the sampling solution (a pediatric catheter connected to a 50-ml syringe
may be used as an alternative to the collector).
6) Alveolar lavage fluid: After local anesthesia, insert a bronchoscope through the mouth or nose,
pass through the pharynx into the branch of the right middle lobe or the lingular segment of the left
lung, and insert the tip into the bronchial branch opening; slowly add sterilized physiological saline
through the biopsy hole of the bronchoscope, with 30-50 ml of saline each time, 100-250 ml in total,
300 ml at most.
7) Fecal specimen: Take 1ml sample treatment solution, pick up a little sample about the size of a
soybean and add it into the tube, gently blow for 3-5 times, set aside at room temperature for 10
minutes, centrifuge at 8,000rpm for 5 minutes, absorb the supernatant for detection.
Fecal specimen treatment solution can be prepared in-house by the laboratory: 1.211g tris, 8.5g
sodium chloride, 1.1 g calcium chloride anhydrous or 1.47g calcium chloride containing crystalline
water, dissolved into 800 ml deionized water, with the pH adjusted to 7.5 with concentrated
hydrochloric acid and replenishing with deionized water to 1000 ml.
Stool suspensions can also be prepared using HANK's solution or other isotonic saline solution, tissue
culture solution or phosphate buffer solution. If the patient has diarrhea symptoms, collect 3-5 ml of
stool specimen, gently blow and mix, centrifuge it at 8,000rpm for 5 minutes, absorb the supernatant
to reserve for use.
8) Anal swab: Gently insert the disinfectant cotton swab into the anus for 3-5cm in depth, then gently
rotate and pull out, immediately put the swab into a 15-ml screw-capped sampling tube containing 3-
5ml virus preservation solution, discard the tail and tighten the tube cover.
9) Blood samples: it is recommended to use vacuum blood vessels containing EDTA anticoagulant to
collect 5ml of blood samples. Nucleic acid extraction should be performed on whole blood or plasma
according to the type of nucleic acid extraction reagent selected. For plasma separation, the whole
blood should be centrifuged at 1,500 to 2,000 rpm for 10 minutes, and the supernatant will be
collected in a in sterile plastic tubes with screw cap.
10) Serum specimen: Collect a 5-ml blood specimen with a vacuum negative-pressure blood collection
tube. Keep the specimen at room temperature for 30 minutes, centrifuge it at 1,500- 2,000 rpm for 10
minutes, and collect the serum in a sterile plastic tube with screw cap.
Other materials: To be collected in a standardized manner in accordance with design requirements.
5. Specimen packaging
Collected specimens shall be packaged separately in a biosafety cabinet of a BSL-2 laboratory.
1) All specimens should be placed in an airtight freeze-tolerant sample collection tube of appropriate
size, with a screw cap and a gasket inside. The sample number, category, name and sampling date
should be indicated on the outside of the container.
2) Specimens kept in an airtight container should be sealed in a plastic bag of appropriate size, with
each bag containing one specimen. The specimen packaging requirements must meet the

corresponding standards of the Technical Regulations for the Safe Transport of Dangerous Goods by
Air.
3) Prior to transportation, external specimens shall undergo the three-layer packaging applicable to
Category A and Category B infectious substances based on the categories of the specimens.
6. Specimen preservation
Specimens for virus isolation and nucleic acid detection purposes should be tested as soon as possible.
Specimens to be tested within 24 hours can be stored at 4 °C; those that cannot be tested within 24
hours should be stored at -70 °C or below (specimens may be temporarily stored in -20 °C refrigerators
in the absence of -70 °C storage condition). Serum can be stored at 4 °C for 3 days and below -20 °C
for a longer period. A special depot or cabinet is required to store specimens separately. Repeated
freeze-thaw cycles during specimen transportation should be avoided.
7. Specimen submission and examination
Collected specimens should be sent to laboratories as soon as possible. Dry ice and other refrigeration
methods are recommended for the preservation of specimens to be transported over long distances.
1) Submission of specimens
Specimens of cluster cases in each province (autonomous region, municipality directly under the
central government) shall be submitted to the National Institute for Viral Disease Control and
Prevention (NIVDC) under China CDC for testing and review, with the specimen submission form
attached (see Appendix).
2) Pathogen and specimen transportation
2.1) Domestic transport
Novel coronavirus strains or other potentially infectious biological substances are subject to the
packaging instructions for Category A substances assigned to UN2814, and the PI 602 of the
Technical Instructions For The Safe Transport of Dangerous Goods by Air (Doc 9284) issued by ICAO;
environmental samples, assigned to UN3373, shall be transported in Category B packaging in
accordance with the PI 650, Doc 9284; one may refer to the aforementioned standards for specimens
to be transported in other modes of transportation.
A Permit of Transport is required for the transportation of the novel coronavirus strains or other
potentially infectious substances, according to the Transport Regulations on the Highly Pathogenic
Microorganism (Virus) Strains and Specimens that are Pathogenic to Humans (Order No. 45, former
Ministry of Health).
2.2) International transport
Standard packaging shall be applied to novel coronavirus strains or samples to be transported
internationally, with relevant procedures handled in accordance with the Provisions on the
Administration of the Health Quarantine of Entry/ Exit Special Articles as well as relevant national and
international requirements.
2.3) Management of strains and samples
Novel coronavirus strains and samples should be managed by designated personnel, with the source,
category, quantity and registration number of the strains and samples recorded accurately. Effective

measures should be adopted to ensure the security of the strains and samples. Efforts should be made
to prevent the misuse, malicious use, theft, robbery, loss, and leakage of the strains and samples.
II Laboratory testing of the novel coronavirus
The conventional testing method for novel coronavirus infection is real-time fluorescence-based RT-
PCR assays. Any test of the novel coronavirus must be performed in a laboratory with appropriate
conditions by personnel trained in relevant technical safety skills. The nucleic acid detection method
introduced in this guideline mainly targets at open reading frame 1ab (ORF lab) and nucleocapsid
protein (N) in the novel coronavirus genome.
To confirm a case as positive in the laboratory, one of the following criteria shall be met:
1. The real-time fluorescence-based RT-PCR assay of the novel coronavirus in the same specimen
shows that the two targets, ORF1ab and Protein N, are both positive. In case of the result showing
positive for one target, then samples shall be re-collected for another test. If it is still positive for a
single target, it is determined to be positive.
2. The real-time fluorescence-based RT-PCR assay of two types of specimens show one single target
positive at the same time, or one target positive in two samples of the same type, it could be
determined as positive.
Negative nucleic acid results cannot rule out novel coronavirus infections. Factors leading to false
negatives shall be precluded, including: poor qualities of samples, for instance the respiratory tract
samples in the oropharynx and other parts; samples collected too early or too late; samples that are
improperly stored, transported or processed; technical reasons such as virus mutations, PCR inhibition,
etc.
III. Real-Time fluorescence-based RT-PCR assay of the novel coronavirus nucleic acid
1. Purpose
To standardize the procedure of testing the novel coronavirus nucleic acid with the real-time
fluorescence-based RT-PCR assay, ensuring correct and reliable test results.
2. Scope
Applicable to the real-time fluorescent RT-PCR assay of the novel coronavirus nucleic acid.
3. Responsibilities
Testing personnel: testing the samples in accordance with this guideline.
Reviewing personnel: reviewing whether the test operations are standardized and whether test results
are accurate or not.
Department head: comprehensively managing the department and reviewing test reports.
4. Sample reception and preparation
Reviewing the name, sex, age, number, and test items of the sample to be tested; indicate any
abnormalities of the testing samples; testing samples shall be stored in a -70 °C refrigerator.
5. Test items
(1) Novel coronavirus nucleic acid assay (real-time fluorescence-based RT-PCR assay)

Primers and probes targeting the ORF1ab and N gene regions of the novel coronavirus are
recommended.
Target 1 (ORF1ab):
Forward primer (F): CCCTGTGGGTTTTACACTTAA
Reverse primer (R): ACGATTGTGCATCAGCTGA
Fluorescent probe (P): 5'-FAM-CCGTCTGCGGTATGTGGAAAGGTTATGG-BHQ1-3'
Target 2 (N):
Forward primer (F): GGGGAACTTCTCCTGCTAGAAT
Reverse primer (R): CAGACATTTTGCTCTCAAGCTG
Fluorescent probe (P): 5'-FAM-TTGCTGCTGCTTGACAGATT-TAMRA-3'
For nucleic acid extraction and real-time fluorescence-based RT-PCR reaction system and reaction
conditions, refer to kit instructions of the manufacturers concerned.
(2) Judgment of results
Negative: no Ct value or Ct value≥ 40.
Positive: Ct value <37.
Gray zone: Repeated experiments are recommended should Ct value range between 37 and 40. If the
Ct value reads <40 and the amplification curve has obvious peaks, the sample should be considered
being tested positive, otherwise it should be considered as negative.
Note: If a commercial kit is used, the instructions provided by the manufacturer shall prevail.
IV. Biosafety requirements for pathogen experiments
According to the biological features, epidemiological characteristics, clinical data and other available
information concerning the novel coronavirus, the pathogen shall be temporally managed as Category
B pathogens and microorganisms based on its hazards. Specific requirements are listed as follows:
1. Viral culture
Viral culture refers to operations such as virus isolation, culture, titration, neutralization test,
purification of live virus and its protein, lyophilization of virus, and recombination test to produce live
virus. The above operations should be performed in a biosafety cabinet of a BSL-3 laboratory. When
viral medium is used to extract nucleic acid, the addition of lysing agent or inactivating agent must be
performed under the same level of laboratory and protective conditions as viral culture. Laboratories
shall report to the National Health Commission for approval and obtain relevant qualifications before
carrying out the corresponding activities.
2. Animal infection experiment
Animal infection experiment refers to operations such as infecting animals with live viruses, sampling
of infected animals, processing and testing of infectious samples, special test for infected animals,
disposal of infected animal excrement, etc., which should be performed in a biosafety cabinet of a BSL-
3 laboratory. Laboratories shall report to the National Health Commission for approval and obtain
relevant qualifications before carrying out the corresponding activities.
3. Operation of uncultured infectious substances

The operation of uncultured infectious substances refers to viral antigen detection, serological testing,
nucleic acid extraction, biochemical analysis, inactivation of clinical samples and other operations
performed on uncultured infectious substances before inactivation through a reliable method. The
operation should be performed in a BSL-2 laboratory, with personal protective equipment subject to
BSL-3 laboratory protection requirements.
4. Operation of inactivated substances
After reliable inactivation of infectious substances or live viruses, operations such as nucleic acid
testing, antigen testing, serological testing and biochemical analysis should be performed in a BSL-2
laboratory. Molecular cloning and other operations not involving live pathogenic viruses may be
carried out in a BSL-1 laboratory.
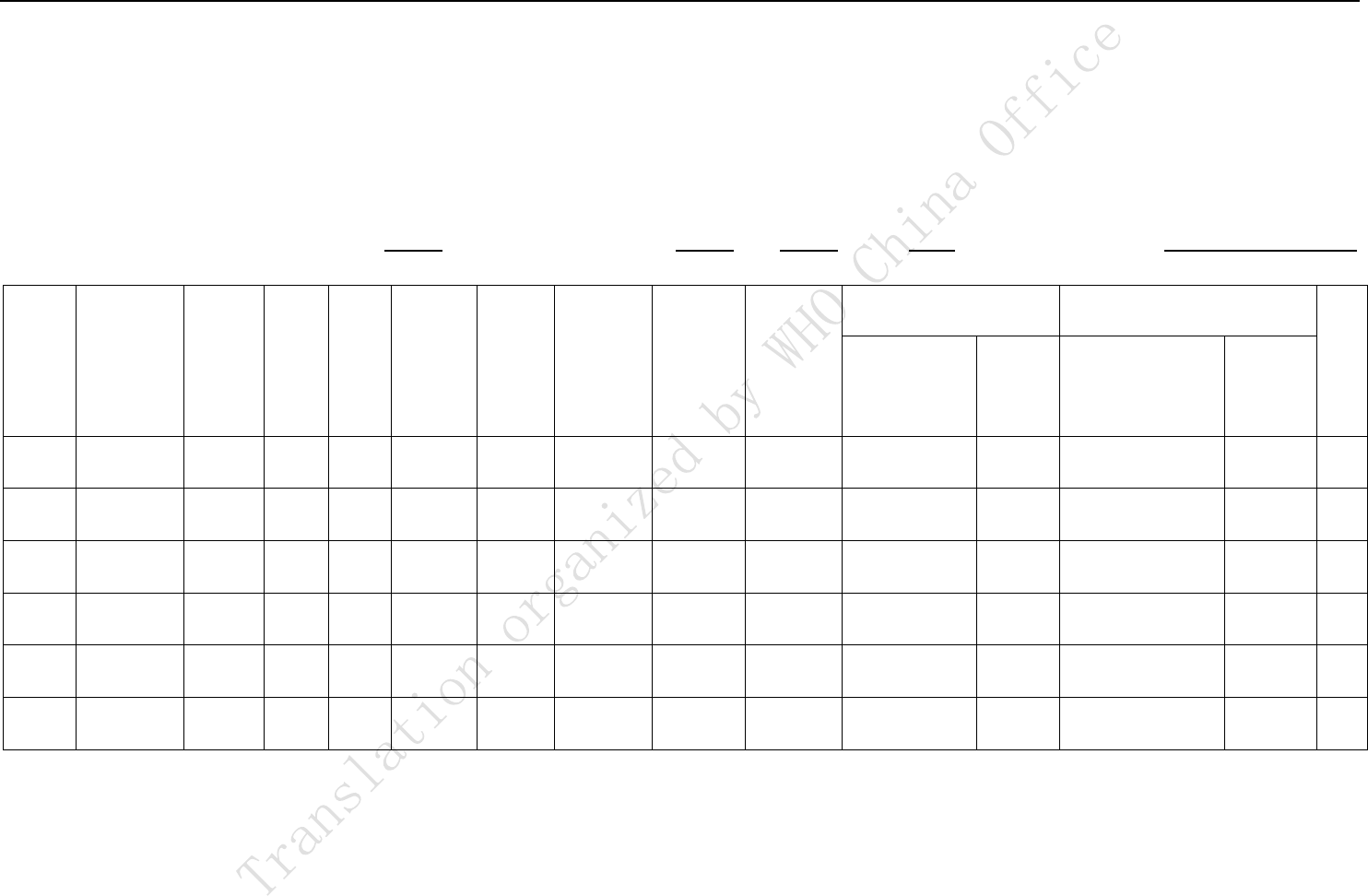
Annex
Novel coronavirus testing
Specimen Submission Form
Specimen submission unit (seal):
Submission date:
year
month
day
Submitted by:
No.
Specimen
type
Name
Sex
Age
Date of
onset
Date of
clinical
visit
Sampling
date
From a
clustered
outbreak
or not
Testing
date
Real-time fluorescent RT-
PCR
Gene sequence homology*
Note
Reagent
manufacturer
Target
gene
First generation
Deep
sequencin
g
Gene sequence homology * is not a required option; it Indicates completion of the specific target gene sequence / whole genome sequence and its homology with the
novel coronavirus. For the column of “from a clustered break or not”, fill in “yes” or “no”.
