ORIGINAL RESEARCH
published: 29 April 2022
doi: 10.3389/fmed.2022.738541
Frontiers in Medicine | www.frontiersin.org 1 April 2022 | Volume 9 | Article 738541
Edited by:
Reza Lashgari,
Shahid Beheshti University, Iran
Reviewed by:
Kuldeep Singh,
National Institute of Malaria Research
(ICMR), India
Gengfeng Fu,
Jiangsu Provincial Center for Disease
Control and Prevention, China
Junjie Wang,
Chinese Center for Disease Control
and Prevention, China
*Correspondence:
Hong Shang
Junjie Xu
†
These authors have contributed
equally to this work
Specialty section:
This article was submitted to
Infectious Diseases–Surveillance,
Prevention and Treatment,
a section of the journal
Frontiers in Medicine
Received: 09 July 2021
Accepted: 28 March 2022
Published: 29 April 2022
Citation:
Gao Y, Hu Q, Leuba SI, Jia L, Wang H,
Huang X, Chen Y, Wang H, Zhang J,
Chu Z, Zhang L, Wang Z, Shang H,
Xu J and CROPrEP Study Team
(2022) Medication Non-adherence
and Condomless Anal Intercourse
Increased Substantially During the
COVID-19 Pandemic Among MSM
PrEP Users: A Retrospective Cohort
Study in Four Chinese Metropolises.
Front. Med. 9:738541.
doi: 10.3389/fmed.2022.738541
Medication Non-adherence and
Condomless Anal Intercourse
Increased Substantially During the
COVID-19 Pandemic Among MSM
PrEP Users: A Retrospective Cohort
Study in Four Chinese Metropolises
Yangyang Gao
1,2,3,4†
, Qinghai Hu
1,2,3,4†
, Sequoia I. Leuba
5
, Le Jia
1,2,3,4
, Hongyi Wang
1,2,3,4
,
Xiaojie Huang
6
, Yaokai Chen
7
, Hui Wang
8
, Jing Zhang
1,2,3,4
, Zhenxing Chu
1,2,3,4
,
Lukun Zhang
8
, Zixin Wang
9
, Hong Shang
1,2,3,4
*
, Junjie Xu
1,2,3,4
*
and CROPrEP Study Team
1
National Health Commission Key Laboratory of Acquired Immunodeficiency Syndrome (AIDS) Immunology (China Medical
University), National Clinical Research Center for Laboratory Medicine, The First Affiliated Hospital of China Medical
University, Shenyang, China,
2
Key Laboratory of AIDS Immunology, Chinese Academy of Medical Sciences,
Shenyang, China,
3
Key Laboratory of AIDS Immunology of Liaoning Province, Shenyang, China,
4
Collaborative Innovation
Center for Diagnosis and Treatment of Infectious Diseases, Hangzhou, China,
5
Department of Epidemiology, U niversity of
North Carolina at Chapel Hill, Chapel Hill, NC, United States,
6
Center for Infectious Diseases, Beijing Youan Hospital, Capital
Medical University, Beijing, China,
7
Chongqing Public Health Medical Center, Chongqing, China,
8
Department of Infectious
Diseases, National Clinical Center for Infectious Diseases, Third People’s Hospital of Shenzhen, Second Affiliated Hospital of
Southern University of Science and Technology, Shenzhen, China,
9
Faculty of Medicine, The Jockey Club School of Public
Health and Primary Care, The Chinese University of Hong Kong, Hong Kong, Hong Kong SAR, China
Background: The coronavirus disease (COVID-19) pandemic has impacted HIV
prevention strategies globally. However, changes in pre-exposure prophylaxis (PrEP)
adherence and HIV-related behaviors, and their associations with medication adherence
among men who have sex with men (MSM) PrEP users remain unclear since the onset
of the COVID-19 pandemic.
Methods: A Retrospective Cohort Study of HIV-negative MSM PrEP users was
conducted in four Chinese metropolises from December 2018 to March 2020, assessing
the changes in PrEP adherence and HIV-related behaviors before and during the COVID-
19. The primary outcome was poor PrEP adherence dete rmined from self-reported
missing at least one PrEP dose in the previous month. We used multivariable logistic
regression to determine factors correlated with poor adherence during COVID-19.
Results: We enrolled 791 eligible participants (418 [52.8%] in daily PrEP and 373
[47.2%] in event-driven PrEP). Compared with the data conducted before the COVID-19,
the proportion of PrEP users decreased from 97.9 to 64.3%, and the proportion of poor
PrEP adherence increased from 23.6 to 50.1% during the COVID-19 [odds ratio (OR)
3.24, 95% confidence interval (CI) 2.62–4.02]. While the percentage of condomless anal
intercourse (CAI) with regular partners (11.8 vs. 25.7%) and with casual partners (4.4

Gao et al. PrEP Adherence During the COVID-19 Pandemic
vs. 9.0%) both significantly increased. The proportion of those who were tested for HIV
decreased from 50.1 to 25.9%. Factors correlated with poor PrEP adherence during the
COVID-19 included not being tested for HIV (adjusted odds ratio [aOR] = 1.38 [95% CI:
1.00, 1.91]), using condoms consistently with regular partners (vs. never, aOR = 2.19
[95% CI: 1.16, 4.13]), and being married or cohabitating with a woman (vs. not married,
aOR = 3.08 [95% CI: 1.60, 5.95]).
Conclusions: Increased poor PrEP adherence and CAI along with the decrease in HIV
testing can lead to an increase in HIV acquisition and drug resistance to PrEP. Targeted
interventions are needed to improve PrEP adherence and HIV prevention strategies.
Keywords: COVID-19, pre-exposure prophylaxis (PrEP), adherence–compliance–persistence, men who have sex
with men (MSM), condomless anal intercourse (CAI)
INTRODUCTION
Since the declaration of the coronavirus disease 2019 (COVID-
19) pandemic by the World Health Organization (WHO) on
11 March 2020, social distancing has interrupted hospital-
based HIV prevention met hods, HIV care, and testing services,
particularly among men who have sex with men (MSM) (
1, 2).
Almost one quarter (23%) of new HIV infections globally in
2019 were among MSM, and the percentage of incident HIV
infections among MSM was even higher in the Asia-Pacific region
(3). The HIV incidence among Chinese MSM has increased from
3.24/100 PY (95% CI: 2.81–3.74) in 2005–2008 to 5.95/100 PY
(95% CI: 5.37–6.56) in 2012–2018 (4). New strategies to prevent
HIV transmission, especially those that are effective despite social
distancing, are needed to address t he increasing HIV epidemic
among Chinese MSM.
Pre-exposure prophylaxis (PrEP) is an innovative and effective
biomedical HIV prevention s trate gy for people at high risk
of HIV infection (
5). PrEP is a medication that is usually
taken daily or event-driven to prevent HIV transmission and
is frequently tenofovir/emtricitabine (TDF/FTC). If used with
optimal adherence, PrEP is highly effective at preventing HIV
transmission (6, 7). However, if adherence is <40%, PrEP is no
longer protective against HIV transmission (8). Since the onset
of the COVID-19 pandemic, few studies have assessed PrEP
adherence but several have reported that the number of PrEP
users has decreased significantly (9, 10). In the United K ingdom,
Belgium, and Australia, there have been 80.0, 47.0, and 4 1.8%
reductions in HIV PrEP users after the outbreak of COVID-
19, respectively (
11–13). In addition to decreasing the use of
PrEP, changes in HIV-related sexual behaviors and increased
barriers to accessing HIV prevention and testing services during
the COVID-19 pandemic could lead to an increase in HIV
acquisition (9, 11, 14). Little is known about possible changes
Abbreviations: COVID-19, coronavirus disease 2019; PrEP, pre-exposure
prophylaxis; MSM, men who have sex with men; OR, odds ratio; CI, confidence
interval; CAI, condomless anal intercourse; WHO, World Health Organization;
PY, person-years; TDF/FTC, tenofovir/emtricitabine; CROPrEP, the China Real-
world Oral Intake of PrEP; IQR, interquartile range; HIVST, HIV self-testing; aOR,
adjusted odds ratio.
in PrEP adherence and HIV-related sexual and testing behaviors
from before to during the COVID-19 pandemic.
This study was based on the China Real-world Oral Intake
of PrEP (CROPrEP) project, which is an ongoing multi-center,
real-world trial of HIV PrEP among Chinese MSM to assess the
effectiveness and adherence of daily or event-driven PrEP (
15).
Participants would complete five follow-up visits that included
an online questionnaire and a clinic visit at 4, 12, 24, 36, and
48 weeks after enrollment. After clinical evaluations and HIV
laboratory testing, participants received TDF/FTC tablets to use
as PrEP. We, thus, investigated PrEP adherence and HIV-related
sexual and testing behaviors among Chinese MSM PrEP users
and determining factors c orrelated with poor adherence before
and during the COVID-19 outbreak. Our findings will help
researchers develop interventions to maintain and support PrEP
use during the pandemic.
METHODS
Study Design
The study recruited 791 MSM aged 16–65 years from four major
Chinese cities (Shenyang, Beijing, Shenzhen, and Chongqing)
from December 2018 to March 2020. In this study, we invited
participants to complete two online self-administered surveys.
The aim of this study was to determine changes in PrEP
adherence and HIV-related and testing behaviors among PrEP-
using Chinese MSM from before to during the COVID-19
outbreak. The median interval between the 4-week visit and
this additional online sur vey was 28 weeks, and the interquartile
range (IQR) was 24–36 weeks.
Participants
The inclusion criteria for this additional online survey were t h e
following: (1) participants of the CROPrEP project, (2) screened
to be HIV-negative at the most recent follow-up visit, and (3)
had not yet completed t he final follow-up visit at Week 48. We
excluded those who did not complete a Week 4 follow-up visit as
data from this visit were used to provide information from before
the COVID-19 outbreak.
Frontiers in Medicine | www.frontiersin.org 2 April 2022 | Volume 9 | Article 738541

Gao et al. PrEP Adherence During the COVID-19 Pandemic
Data Collection
This additional online survey assessing changes in PrEP
adherence and HIV-related sexual and testing behaviors due to
the COVID-19 pandemic was developed by a panel consisting of
HIV epidemiologists, clinicians, and MSM-serving community-
based organization members. This questionnaire was then pilot-
tested among 15 MSM volunteers who were not CROPrEP
participants and was revised based on their comments. A link
to this additional online questionnaire was shared among all
participants in CROPrEP by using the WeC hat (i.e., a popular
social media platform) group. If participants did not complete
the survey within 24 h, project staff reminded them of the
invitation v ia a phone call or a text message. Participation in
this additional online survey was voluntary, refusal to participate
had no effect on their participation in the CROPrEP project,
and data were confidential and used only for research purposes.
Each individual account was allowed to access the online
questionnaire only once to avoid duplicate responses (refer to
Supplementary Appendix 1).
Measures
Before the COVID-19, measures were determined from the 4-
week follow-up visit for CROPrEP, conducted between October
2018 and November 2019, and during the COVID-19, measures
were determined from the additional online survey conducted
between February and March 2020. Baseline background
characteristics assessed included type of PrEP regimen, age,
education, monthly income, marital status, sexual identity, and
lockdown restrictions experience (during the COVID-19 survey
only). We asked about HIV-related sexual behaviors, such as
primary locations to seek male sexual partners, the number
and types of male sexual partners, frequency of sexual acts,
frequency of condomless anal intercourse (CAI) with s pecific
types of male sexual partners, and sexualized drug use. For
HIV testing behavior, we asked about the self-perceived risk of
HIV infection, H IV test behavior in the past month, location
of the HIV test [i.e., facility-based HIV testing or HIV self-
testing (HIVST)], and self-assessment of the frequency of HIV
testing compared with pre-COVID-19 (during the COVID-19
survey only). To assess changes, we also asked whether they
had experienced lockdown restrictions due to COVID-19, how
frequently were they concerned about the COVID-19 pa ndemic
(i.e., never, sometimes, often, and always), or whether they had
delayed a scheduled follow-up visit for the CROPrEP project
(refer to Supplementary Appendix 2).
Male sexual partners were defined as regular (i.e., those who
were in a stable relationship and did not involve transactional
sex) or casual (i.e., those who were not in a stable relationship
and did not involve transactional sex). Sexualized drug use
was defined as using any of the following drugs during sexual
relations in the previous month: rush poppers (alkyl nitrites),
cocaine, methamphetamine, ketamine, and bath salts. Having
delayed a scheduled follow-up visit for the CROPrEP project
was defined as attending a follow-up visit after the previously
scheduled appointment date by 7 days or more.
Outcome
Self-reported PrEP adherence was defined based on a
comprehensive evaluation of the self-reported missed PrEP
doses and sexual behaviors. Poor adherence was defined as the
following: (1) missing doses among daily PrEP users in the past
month and (2) missing doses among event-driven PrEP users if
they had sexual behaviors in the past month. If not defined as
having poor adherence, participants were defined as having good
adherence during the COVID-19 (
16).
Statistical Analysis
We analyzed the demographics and HIV-related behaviors of
Chinese MSM PrEP users using frequencies and percentages.
We then used the generalized estimating equation (GEE model-
Binary logistic regression) to analyze the changes in adherence
and HIV-related behaviors sexual and testing behaviors, and
PrEP use in the past month from before (using data from the
4-week follow-up visit from CROPrEP) and during the COVID-
19 outbreak (using data collected from the additional online
survey during COVID-19). We then assessed factors correlated
with poor adherence using univariable and multivariable logistic
regression models adjusted for age, education, and monthly
income. A two-tailed value of p below 0.05 and between 0.05
and 0.10 was considered statistically significant and marginally
significant, respectively. All statistical analyses were performed
using SPSS
TM
software version 25.0 (IBM Corp, Armonk,
NY, US).
Ethical Review
This study was reviewed and approved by the Medical Science
Research Ethics Committee of the First Affiliated Hospital of
China Medical University ([2018]2015-139-5) and was registered
with the Chinese Clinical Trial Registry (C hiCTR-IIN-17013762).
After providing online informed consent, eligible participants
were asked to complete the additional questionnaire and had
the opportunity to review and modify their responses. All data
and informed consent were password-protected a nd stored in
a secure server, and only the principal investigator had access
to the database. E ach participant was compensated $4.20 (30
Yuan) after completing the additional online survey (refer to
Supplementary Appendix 3).
RESULTS
Baseline Characteristics
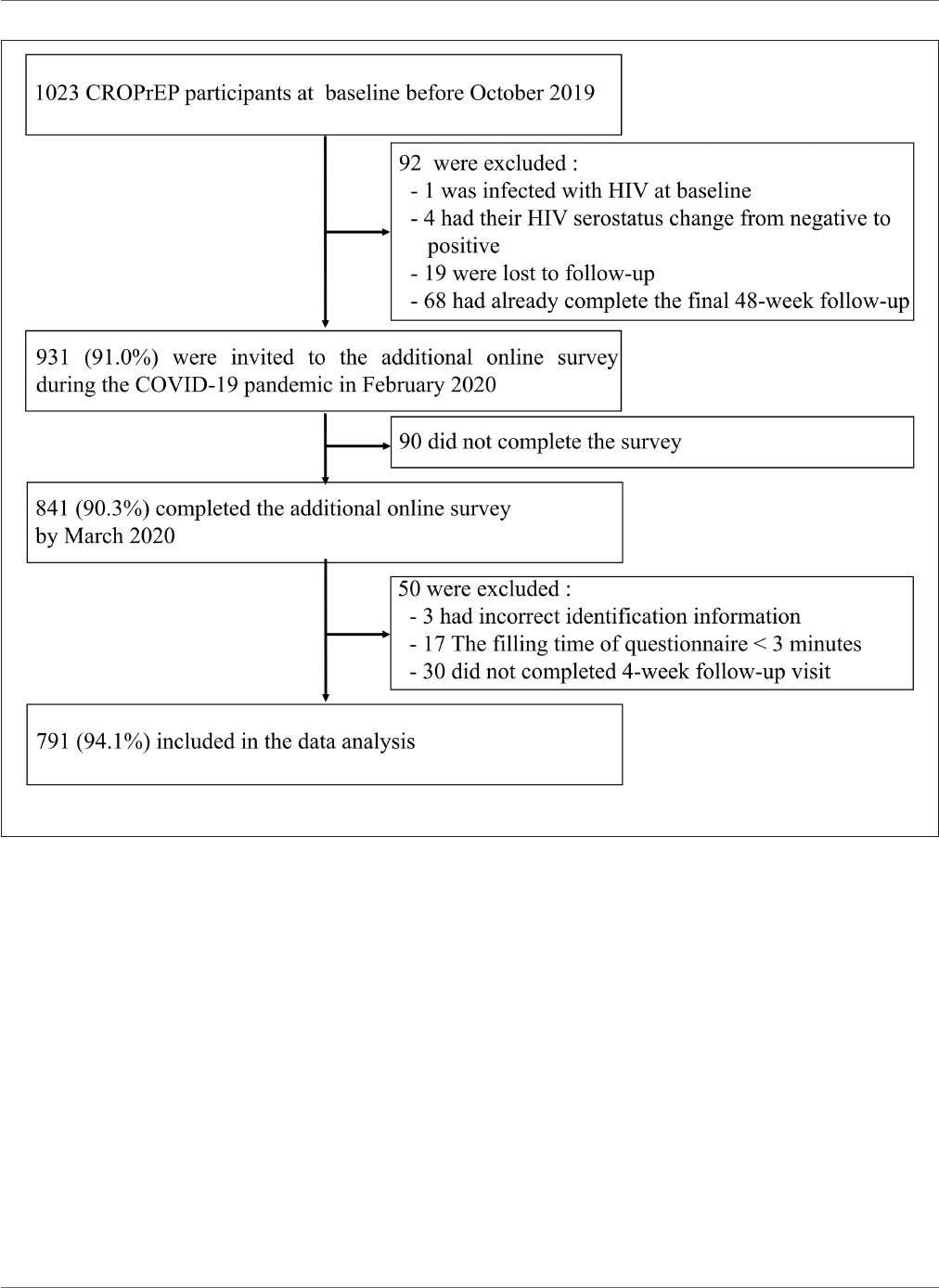
Before the COVID-19 outbreak, 1,023 MSM were enrolled in
the CROPrEP trial, and 931 (91.0%) were invited to participate
in this survey. During the COVID-19 pandemic, 841 (90.3%)
invited participants completed the online survey, and of these
participants, 791 (9 4.1%) were included in the data analysis
(300 in Shenyang, 362 in Beijing, 61 in Shenzhen, and 68 in
Chongqing) (refer to Figure 1). The median age of participants
was 30 years (IQR: 26–36 years), 79.6% (630/791) had an
education level of college and above, 38.1% (301/791) had a
monthly income of 2,001–6,000 Yuan (∼$310–92 9), and 81.0%
(641/791) self-described their sexual identity as a homosexual. In
response to COVID-19, 93.6% (740/791) of participants reported
Frontiers in Medicine | www.frontiersin.org 3 April 2022 | Volume 9 | Article 738541
Gao et al. PrEP Adherence During the COVID-19 Pandemic
FIGURE 1 | Study profile.
experiencing COVID-19 lockdown restrictions, such as physical
distancing, community restrictions, and the banning of indoor
gatherings (refer to Table 1).
Changes in HIV-Related Sexual Behavior,
HIV Testing, and PrEP Adherence From
Before to During the COVID-19 Pandemic
Sexual acts, sexualized drug use, HIV testing, and PrEP use
and adherence sharply decreased as more participants had no
partner during the pandemic. The percentage of participants
who had regular or no male sexual partners in the past month
greatly increased from 33.4% (264/791) before to 74.0% (585/791)
during COVID-19, and the percentage of those who used the
internet as their primary location to seek male sexual partners
dropped from 60.4% (478/7 91) before to 25.3% (200/791) during
COVID-19. In addition, sexual activity, such as frequency of
sexual acts, having 2 or more male sexual partners and having
either a regular or casual male s exual partner greatly decreased
from before to during COVID-19. However, the proportion
of CAI with regular (11.8–25.7%) and casual (4.4–9.0%) male
sexual partners incre ased during COVID-19. Sexualized drug
use sharply decreased from 39.8% (315/791) before to 24.1%
(191/791) during COVID-19. HIV testing behaviors sharply
decreased from 50.1% (396/791) of participants having been
tested for HI V in the past month before COVID-19 to
25.9% (205/791) during COVID-19, including HIVST (34.5%
(273/791) before to 20.7% (164/791) during COVID-19) or
through a facility [26.9% (213/791) before to 6.4% (51/791)
during COVID-19]. Prevention of HIV also decreased as PrEP
use dropped from 97.9% (774/791) before to 64.5% (510/791)
and poor PrEP adherence increased from 23.6% (187/791)
before to 50.1% (396/791) during COVID-19. Participants also
delayed a scheduled follow-up visit for the CROPrEP trial more
during COVID-19 (14.5%, 115/791) than before (10.0%, 79 /791)
(refer to Table 2).
Frontiers in Medicine | www.frontiersin.org 4 April 2022 | Volume 9 | Article 738541

Gao et al. PrEP Adherence During the COVID-19 Pandemic
TABLE 1 | Characteristics of Chinese MSM PrEP users during the COVID-19
pandemic (N = 791).
Characteristic Participants (n, %)
PrEP regimen
Daily 418 (52.8)
Event-driven 373 (47.2)
Age (years)
18-24 130 (16.4)
25-39 534 (67.5)
40-65 127 (16.1)
Education
High school and below 161 (20.4)
College and above 630 (79.6)
Average monthly income (RMB, Yuan)
<2,000 129 (16.3)
2,001-6,000 301 (38.1)
6,001-10,000 153 (19.3)
More than 10,000 208 (26.3)
Marital status
Not married 499 (63.1)
Married or cohabitating with a woman 61 (7.7)
Cohabitating with a male 203 (25.7)
Divorced, separated, or widowed 28 (3.5)
Sexual identity
Homosexual 641 (81.0)
Bisexual 126 (15.9)
Heterosexual 3 (0.4)
Not sure 21 (2.7)
Experienced lockdown restrictions in response to COVID-19*
Yes 740 (93.6)
No 51 (6.4)
Data are from the additional online survey administered during the COVID-19 pandemic.
MSM, men who have sex with men; PrEP, pre-exposure prophylaxis; COVID-19,
Coronavirus disease 2019.
*
Lockdown restrictions include physical distancing of two meters when individuals have
to leave their homes, community restrictions, and the banning of indoor gatherings.
In the generalized estimating equations model, there was a
significant decrease in the odds of using PrEP (odds ratio (OR)
= 0.04 [95% CI: 0.02, 0.07], p < 0.001) and a significant increase
in the odds of self-reporting missing at le ast one PrEP dose (O R =
3.24 [95% CI: 2.62, 4.02], p < 0.0 01) and in the odds of delaying a
scheduled CROPrEP follow-up visit (OR = 1.54 [95% CI: 1.13,
2.08], p = 0.006) compared during to before the COVID-19
pandemic. Additionally, there were significant reductions in the
odds of having been tested for HIV in the past month (OR = 0.3 5
[95% CI: 0.28, 0.43], p < 0 .001) . In concordance with the decrease
in HIV-related sexual behavior, there was a significant increase
in the odds of self-perceiving risk of HIV infection as compared
with no risk (OR = 3.41 [95% CI: 2.72, 4.28], p < 0. 001). By
contrast, among those still having sexual behavior during the
COVID-19, there were signific ant increases in the odds of having
CAI wit h regular male sexual partners (OR = 2.61 [95% CI: 1.76,
2.87], p < 0.001) and marginal increases in the odds of having
CAI with casual male sexual partners (OR = 2.09, 95% CI: 0.92,
4.72, p = 0.077) compared to before COVID-19 (refer to Table 2).
Factors Correlated With Poor PrEP
Adherence During the COVID-19 Pandemic
About half of the participants (396/791, 50.1%) were defined
as having poor PrEP adherence during the COVID-19. After
adjusting for age, education, and income, the following factors
over the past month were associated with increased odds of poor
PrEP adherence during the COVID-19 pandemic: being married
or cohabitating with a woman (compared with not married:
aOR = 3.08 [95% CI: 1.60, 5.95], p < 0.001), using condoms
consistently with regular male sexual partners (compared with
never using condoms: aOR = 2.1 9 [95% CI: 1.16, 4.13], p =
0.016), and often concerned about the COVID-19 pandemic
(compared with always concerned: aOR = 1.45 [95% CI: 1.07,
1.97], p = 0.017). Knowing the HIV status of regular male sexual
partners (aOR = 1.44 [95% CI: 0.98, 2.11], p = 0.065) and not
having been tested for HIV in the previous month (compared
with have been tested for HIV: aOR = 1.38 [95% CI: 1.00–1.91],
p = 0.050) were associated with marginally higher odds of poor
PrEP adherence. There was no difference in the odds of poor or
good PrEP adherence based on the PrEP dosing regimen (event-
driven vs. daily: aOR = 1.09 [95% CI: 0.82, 1.45], p = 0.560) (refer
to Table 3).
DISCUSSION
In this retrospective cohort study in China, we found a dramatic
increase in poor PrEP adherence along with decreases in HIV
testing, the number of male sexual partners, and sexual acts
during the COVID-19 pandemic. Factors correlated with the
increased odds of poor PrEP adherence during COVID-19
included not having an HIV test conducted in the last month,
using condoms consistently with regular male sexual partners,
and being married or cohabitating with a woman. Among those
who had regular or casual male sexual partners, the percentage
of those who had CAI subst antia lly increased during COVID-
19 compared with the percentage before the pandemic. This
may result in an increased risk of HIV infection and drug
resistance in this sexually active group during the pandemic.
Thus, public health officials should promote safer sex behaviors
among those who are sexually active during COVID-19. In
addition, poor PrEP adherence during the pandemic was found
among participants wit h likely less access to MSM-specific HIV
care, such as MSM married or cohabitating with a woman and
MSM who had not been tested for HIV in the last month. To
improve PrEP adherence, public health officials must improve
outreach to these subpopulations, such as sending at-home HIV
tests, re-inforcing risks for HIV acquisition if poor adherence
to PrEP, and if poor adherence is likely to continue, suggesting
stopping PrEP use to prevent drug resistance. Knowledge about
challenges to PrEP use due to COVID-19 provides first-hand
real-world evidence of issues that must be addressed prior to
wide-spread PrEP implementation globally.
Frontiers in Medicine | www.frontiersin.org 5 April 2022 | Volume 9 | Article 738541
Gao et al. PrEP Adherence During the COVID-19 Pandemic
TABLE 2 | Changes in sexual behaviors, HIV testing, and PrEP adherence among during compared to before the COVID-19 (N = 791).
Before COVID−19
a
During COVID−19 Odds ratio P-value
n (%) n (%) (95% CI)
HIV–related sexual behaviors in the past month
Primary location to seek male sexual partners
Internet 478 (60.4) 200 (25.3) 0.22 (0.18, 0.27) <0.001
Park/Bathroom/Club 49 (6.2) 6 (0.8) 0.12 (0.05, 0.27) <0.001
Had regular or no male sexual partners 264 (33.4) 585 (74.0) 5.68 (4.60, 701) <0.001
Frequency of sexual acts
b
More than once a week 413 (52.2) 125 (15.8) 0.17 (0.14, 0.21) <0.001
Once a week or less than once a week 321 (40.6) 224 (28.3) 0.58 (0.47, 0.72) <0.001
No sex 57 (7.2) 442 (55.9) 16.31 (12.04, 22.10) <0.001
Sexual partners in the past month
Had two or more male sexual partners 536 (67.8) 136 (17.2) 0.10 (0.08, 0.12) <0.001
Had regular male sexual partners 467 (59.0) 249 (31.5) 0.32 (0.26, 0.39) <0.001
Had casual male sexual partners 317 (40.1) 134 (16.9) 0.30 (0.24, 0.38) <0.001
Condom use with regular male sexual partners
c
Consistently 220 (47.1) 121 (48.6) 1.05 (0.79, 1.44) 0.745
Most or sometimes 192 (41.1) 64 (25.7) 0.05 (0.36, 0.70) <0.001
Never 55 (11.8) 64 (25.7) 2.61 (1.76, 2.87) <0.001
Condom use with casual male sexual partners
c
Consistently 167 (52.7) 74 (55.2) 1.13 (0.75, 1.71) 0.566
Most or sometimes 136 (42.9) 48 (35.8) 0.73 (0.348, 1.11) 0.143
Never 14 (4.4) 12 (9.0) 2.09 (0.92, 4.72) 0.077
Sexualized drug use
d
315 (39.8) 191 (24.1) 0.21(0.17, 0.26) <0.001
HIV testing behaviors in the past month
Had HIV test 396 (50.1) 205 (25.9) 0.35 (0.28, 0.43) <0.001
Had HIV test through HIVST 273 (34.5) 164 (20.7) 0.50 (0.40, 0.61) <0.001
Had facility–based HIV testing 213 (26.9) 51 (6.4) 0.19 (0.13, 0.26) <0.001
PrEP status in the past month
PrEP regimen
Daily 410 (51.8) 418 (52.8) 1.04 (0.86, 1.26) 0.682
Event-driven 381 (48.2) 373 (47.2) 0.96 (0.79, 1.17) 0.682
Used PrEP 774 (97.9) 510 (64.5) 0.04 (0.02, 0.07) <0.001
Poor PrEP adherence 187 (23.6) 396 (50.1) 3.24 (2.62, 4.02) <0.001
Delayed scheduled CROPrEP follow–up visit 79 (10.0) 115 (14.5) 1.54 (1.13, 2.08) 0.006
Self–perceived risk of HIV infection
No risk 160 (20.2) 367 (46.4) 3.41 (2.72, 4.28) <0.001
Low risk (<25%) 419 (53.0) 315 (39.8) 0.59 (0.48, 0.72) <0.001
Moderate risk (25–49%) 142 (18.0) 68 (8.6) 0.43 (0.32, 0.58) <0.001
High risk (50–75%) 52 (6.6) 24 (3.0) 0.45 (0.27, 0.72) 0.001
Very high risk (>75%) 18 (2.3) 17 (2.1) 0.94 (0.49, 1.82) 0.862
ALL data are among Chinese MSM PrEP users.
COVID-19, coronavirus disease 2019; MSM, men who have sex with men; PrEP, pre-exposure prophylaxis; HIVST, HIV self-testing.
CROPrEP, China Real-world Oral Intake of PrEP.
a
Before COVID-19 estimates were determined from the 4th week follow-up visit of the China Real-world Oral Intake of PrEP (CROPrEP) project conducted between October 2018 to
November 2019.
b
Sexual acts included receptive anal intercourse, insertive anal intercourse, and oral intercourse.
c
Only people with regular or casual partners answered the question.
d
Sexualized drug use in the past month included use of rush poppers (alkyl nitrites), cocaine, methamphetamine, ketamine, and bath salts before or during sexual activity.
In this study, similar to peer studies finding decreases in the
number of sexual partners and sexual practices since the onset
of COVID-19 (
10, 14, 17), we observed that 93.5% of Chinese
MSM PrEP users were impacted by lockdown restrictions and
had fewer sexual partners and fewer sexual acts. These decreases
may suggest t hat our participants overall may have temporarily
lower risks of HIV infection. Nevertheless, no excess risks among
MSM PrEP users were found in developing countries before.
Frontiers in Medicine | www.frontiersin.org 6 April 2022 | Volume 9 | Article 738541

Gao et al. PrEP Adherence During the COVID-19 Pandemic
TABLE 3 | Factors correlated with poor adherence to PrEP among Chinese MSM PrEP users during the COVID-19 (N = 791).
Poor adherence Good adherence Odds ratio Adjusted odds ratio P-value
n = 396, n (%) n = 395, n (%) (95% CI) (95% CI)
a
PrEP regimen
Event-driven 192 (48.5) 181 (45.8) 1.11 (0.84, 1.47) 1.09 (0.82, 1.45) 0.560
Daily 204 (51.5) 214 (54.2) Reference Reference
Marital status
Married or cohabitating with a woman 45 (11.4) 16 (4.1) 3.10 (1.70, 5.63) 3.08 (1.60, 5.95) 0.001
Cohabitating with male 98 (24.7) 105 (26.6) 1.03 (0.74, 1.43) 1.00 (0.72, 1.40) 0.973
Divorced, separated, or widowed 15 (3.8) 13 (3.3) 1.36 (0.64, 2.88) 1.43 (0.64, 3.18) 0.382
Not married 238 (60.1) 261 (66.1) Reference Reference
Primary location to seek male sexual partners
No male sexual partner 197 (49.7) 173 (43.8) 1.48 (1.05, 2.09) 1.47 (1.04, 2.09) 0.030
Park/Bathroom/Club 3 (0.8) 3 (0.8) 1.30 (0.26, 6.59) 1.02 (0.20, 5.26) 0.985
Had regular male sexual partners 109 (27.5) 106 (26.8) 1.34 (0.91, 1.97) 1.27 (0.86, 1.88) 0.224
Internet
b
87 (22.0) 113 (28.6) Reference Reference
HIV–related sexual behaviors in the past month
Had two or more male sexual partners
Yes 65 (16.4) 71 (18.0) 0.90 (0.62, 1.30) 0.83 (0 .57, 1.20) 0.333
No 331 (83.6) 324 (82.0) Reference Reference
Had regular male sexual partners
Yes 130 (32.8) 119 (30.1) 1.13 (0.84, 1.53) 1.07 (0.79, 1.45) 0.665
No 266 (67.2) 276 (69.9) Reference Reference
Had casual male sexual partners
Yes 61 (15.4) 73 (18.5) 0.80 (0.55, 1.17) 0.79 (0 .55, 1.15) 0.224
No 335 (84.6) 322 (81.5) Reference Reference
Condom use with regular male sexual partners
Consistently 71 (54.6) 50 (42.0) 2.22 (1.19, 4.11) 2.19 (1.16, 4.13) 0.016
Most or sometimes 34 (26.2) 30 (25.2) 1.77 (0.88, 3.57) 1.74 (0.84, 3.61) 0.135
Never 25 (19.2) 39 (32.8) Reference Reference
Condom use with casual male sexual partners
Consistently 34 (55.7) 40 (54.8) 0.85 (0.25, 2.88) 0.96 (0.28, 3.35) 0.951
Most or sometimes 21 (34.4) 27 (37.0) 0.78 (0.22, 2.76) 0.82 (0.23, 3.00) 0.769
Never 6 (9.8) 6 (8.2) Reference Reference
Know the HIV status of regular male sexual partners
Yes 95 (39.4) 72 (30.9) 1.46 (1.00, 2.13) 1.44 (0 .98, 2.11) 0.065
No 146 (60.6) 161 (69.1) Reference Reference
HIV testing behaviors in the past month
Had HIV test
No 304 (76.8) 282 (71.4) 1.32 (0.96, 1.82) 1.38 (1.00, 1.91) 0.050
Yes 92 (23.2) 113 (28.6) Reference Reference
Self–assessment of the frequency of HIV testing
compare to pre-COVID-19
Increase 6 (1.5) 7 (1.8) 0.93 (0.31, 2.79) 0.87 (0.29, 2.66) 0.809
Decrease 111 (28.0) 86 (21.8) 1.40 (1.00, 1.93) 1.46 ( 1.05, 2.03) 0.026
No change 279 (70.5) 302 (76.5) Reference Reference
Concerned about the COVID−19 pandemic
c
Never 2 (0.5) 1 (0.3) 2.52 (0.23, 28.09) 2.90 (0.25, 33.44) 0.393
Sometimes 59 (14.9) 44 (11.1) 1.69 (1.08, 2.65) 1.74 (1.11, 2.75) 0.017
Often 193 (48.7) 171 (43.3) 1.42 (1.05, 1.92) 1.45 (1.07, 1.97) 0.017
Always 142 (35.9) 179 (45.3) Reference Reference
COVID-19, coronavirus disease 2019; MSM, men who have sex with men; PrEP, pre-exposure prophylaxis.
a
Adjusted odds ratios were obtained through multivariable analysis and were adjusted for age, education, and monthly income.
b
Internet include geosocial networking applications including WeChat, QQ, Blued or Jacked.
c
Concerned about the COVID-19 pandemic was defined as how often obtaining information about COVID-19 through social media and other material proactively.
Frontiers in Medicine | www.frontiersin.org 7 April 2022 | Volume 9 | Article 738541

Gao et al. PrEP Adherence During the COVID-19 Pandemic
However, compared with those sexually active individuals before
the pandemic, among those who were sexually active during
the pandemic, a much higher percentage had CAI with sexual
partners. PrEP cannot be used to replace condoms completely
and is a part of a comprehensive prevention strategy that
includes counseling and behavioral interventions promoting
condom use, abstinence, and monogamy (18, 19). An online
survey among MSM from the United States found conflicting
results and did not find an effect on condom use during
COVID-19 (20). A possible explanation is that China was the
first country impacted by COVID-19 and quickly introduced
physical distancing restrictions and lockdowns, leading to sudden
significant changes in lifestyle and sexual practices, while other
countries c ould have anticipated potential restrictions based on
news from China. In the future, public health officials must target
individuals who are likely to maintain sexual activity during
times where general sexual activity drops and promote safer
sex, such as high PrEP adherence and condom use. In addition,
we strongly recommend that medical staff and community
volunteers popularize safety knowledge regularly and emphasize
the significance of PrEP good adherence.
As suboptimal PrEP adherence will decrease the effectiveness
of PrEP (
21), hence, all global public health sections highlight the
importance of maintaining high medication adherence among
subjects who take oral PrEP pills before or after the COVID-19
era. We found worse adherence during COVID-19 as more t han
one-third (35.7%) of participants did not obtain PrEP refills, and
a half (50.1%) self-reported missing at least one PrEP dose in the
previous month. Our findings are similar to the incre ase in the
proportion who discontinued PrEP use and the increase in the
mean number of missed PrEP doses found among MSM in the
Southern United States (
22). I ndividuals may have discontinued
PrEP use because they were no longer engaging in sexual activity
since COVID-19. Among those still engaging in sexual activity,
they could have been unable to access PrEP and thus had
worse adherence because they could not access PrEP or PrEP
support when facilities were closed due to lockdowns. If users
discontinued using PrEP, public he alth officials should reach out
frequently to see if t he y would like to begin using PrEP again,
and if users had worse adherence to PrEP, practitioners should
ensure access to medication through a no-contact method, such
as the mail and counsel users on the importance of adherence to
prevent HIV transmission.
Frequent HIV testing can also help prevent HIV transmission,
but during the COVID-19 pandemic, the rate of HIV testing was
substantially reduced and correlated with poor PrEP adherence
among C hinese MSM PrEP users. Our finding of less HIV
testing, both HIVST and facility-based HIV-testing, was similar
to results from other studies (
23, 24). An online survey from
the Southern United States also found that one-quarter of MSM
PrEP users encountered obstacles to HIV testing (22). These
difficulties in accessing HIV testing could have been caused by
the physical distancing restrictions in response to COVID-19 and
thus restricting access to facility-based HIV testing. However,
continuous use of PrEP pills when infected with HIV can lead
to HIV drug resistance events (
25, 26), and PrEP users must
be tested for HIV at frequent intervals. More web-based health
promotion (e.g., text messaging) and home-based HIV-testing
(e.g., oral self-tests) were practical tools for raising awareness
of sexual health and HIV-testing in the United Kingdom and
Africa (
27, 28). Thus, to flatten the curve of the COVID-19
pandemic, we suggest providing counseling and HIVST through
a no-contact method to PrEP users to ensure timely knowledge
of HIV serostatus and prevent HIV drug resistance.
Along with decreased HIV testing, using condoms
consistently with regular male sexual partners was significantly
correlated with increased odds of poor PrEP adherence during
COVID-19. Consistent with our results, low PrEP ad h erence in
East Africa was associated with using condoms with all types of
partners (
29). We additionally found a decrease in self-perceived
risk of HIV acquisition among PrEP users during COVID-19,
which may be from decreased sexual activity or using condoms
consistently with regular male sexual partners.
In addition to consistent condom use with regular male
sexual partners, being married or cohabitating with a woman
was also correlated with poor PrEP adherence during COVID-
19. Due to traditional Chinese culture and attitudes toward
homosexuality, up to 25–35% of Chinese MSM have already been
in a heterosexual marriage and more than 70% of MSM may
eventually form a family with a woman to have children and help
conceal their homosexuality (
30). Similarly, MSM partnering
with a woman for cultural reasons also occurs in Nigeria and
India (31, 32). However, despite this common practice, little
is known about MSM who are married or cohabiting with a
woman and their adherence to PrEP. It is possible that these
partnered MSM feared disclosure of their PrEP use and, thus,
sexual orient ati on, leading to poor PrEP adherence. Discrete yet
effective strategies are needed to improve PrEP adherence among
MSM married or cohabitating with a woman.
Strengths and Limitations
By surveying changes in PrEP adherence and HIV-related
behaviors from before to during the COVID-19 pandemic from a
large population of Chinese MSM who used PrEP in four Chinese
cities, our results were more representative. We were additionally
able to stratify differences in adherence during the COVID-
19 by PrEP re gimen and found no difference in ad h erence
between them. By being the first study to identify changes in
PrEP adherence and HI V-related behaviors among Chinese MSM
from before to during the COVID-19 pandemic, we were able
to determine obstacles to PrEP adherence due to lockdown that
must be addressed in possible future societal restrictions. A
limitation of this study was that it used self-reported me asures
to define PrEP adherence. Another limitation was that we asked
sensitive questions about sexual activities and our data may
have been influenced by social desirability bias. To address this
issue, the survey was conducted online, was self-reported, and
was anonymous.
CONCLUSION
We demonstrated a substantial increase in poor adherence and
CAI among those sexually active, and a decrease in HIV testing
among Chinese MSM who used PrEP from before to during
Frontiers in Medicine | www.frontiersin.org 8 April 2022 | Volume 9 | Article 738541

Gao et al. PrEP Adherence During the COVID-19 Pandemic
the COVID-19 pandemic. Our results suggest that some MSM
PrEP users have a likely increased risk of HIV acquisition during
COVID-19, and health workers should develop online targeted
interventions, such as adding online follow-up, promoting safer
sex, PrEP adherence, and condom use, providing no-contact
counseling and HIVST to increase knowledge of HIV serostatus,
and prevent drug resistance event to PrEP, and dis cret e strategies
to reach out to MSM married or living with a woman to promote
PrEP adherence.
DATA AVAILABILITY STATEMENT
The datasets presented in this study can be found in online
repositories. The names of the repository/repositories
and accession number(s) can be found in the
article/Supplementary Material.
ETHICS STATEMENT
This study was reviewed and approved by the Medical Science
Research Ethics Committee of the First Affiliated Hospital
of China Medic a l University ([2018]2015-139-5) and was
registered with the Chinese Clinical Trial Registry (ChiCTR-
IIN-17013762). The patients/participants provided their written
informed consent to participate in this study.
CROPrEP STUDY TEAM
Members of the CROPrEP study team not included in the
authors’ list include, Xiaoqing He, Yao Li, Fang Zhao, Yijun Duan,
Rui Li, Shangcao Li, Hang Li, Zhili Hu, Rantong Bao, Sitong Cui,
Zhaozhen Liu, Zehao Ye, and Xiaoyun Shi.
AUTHOR CONTRIBUTIONS
YG conceived and designed the study and analyzed the data. LJ,
QH, HoW, XH, YC, HuW, LZ and ZC performed the study.
YG, QH, and SL draw the figures and tables. YG, QH, ZW, and
SL wrote and revised the manuscript. All authors reviewed and
approved t he final manuscript.
FUNDING
This study was supported by the Mega-Projects of National
Science Research for the 13th Five-Year Plan [2017ZX10201101],
the National Natural Science Foundation of China
[81872674], and the National Science and Technology Major
Project [2018ZX10101001-001-003].
ACKNOWLEDGMENTS
We thank the MSM who participated in this study and the staff of
community-based organizations who contributed to its success.
SUPPLEMENTARY MATERIAL
The Supplementary Material for this article can be found
online at: https://www.frontiersin.org/articles/10.3389/fmed.
2022.738541/full#supplementary-material
REFERENCES
1. World Health Organization. WHO Announces the COVID-19
Outbreak a Pandemic. (2020). Available online at: http://www.
euro.who.int/en/health-topics/health-emergencies/coronavirus-
covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-
\relax$\@@underline\hbox{pandemic}\mathsurround\z@$\relax,2020
(accessed November 26, 2020).
2. Jiang H, Zhou Y, Tang W. Maintaining HIV care during the COVID-19
pandemic. Lancet HIV. (2020) 7:e308-9 . doi: 10.1016/S2352-3018(20)30105-3
3. Joint United Nations Programme on HIV/AIDS, 2020 DATA. (2020). Available
online at: https://aidsinfo.unaids.org/ (accessed November 26, 2020).
4. Joint United Nations Programme on HIV/AIDS, UNAIDS Epidemiological
Estimates. (2020). Available online at: https://aidsinfo.unaids.org/ (accessed
September 29, 2020).
5. McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson
R, et al. Pre-exposure prophylaxis to prevent the acquisition of
HIV-1 infection (PROUD): effectiveness results from the pilot
phase of a pragmatic open-label randomised trial. Lancet. (2016)
387:53–60. doi: 10.1016/S0140-6736(15)00056-2
6. Molina JM, Capitant C, Spire B, Pialoux G, Cotte L, Charreau I, et al. On-
demand preexposure prophylaxis in men at high risk for HIV-1 infection. N
Engl J Med. (2015) 373:2237–46. doi: 10.1056/NEJMoa1506273
7. Molina JM, Charreau I, Spire B, Cotte L, Chas J, Capitant C, et al. Efficacy,
safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis
for HIV in men who have sex with men: an observational cohort study. Lancet
HIV. (2020) 4:e402-10. doi: 10.1016/S2352-3018(17)30089-9
8. Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G,
et al. Tenofovir-based preexposure prophylaxis for HIV infection among
African women. N Engl J Med. (2015) 372: 509–18. doi: 10.1056/NEJMoa
1402269
9. Hammoud MA, Grulich A, Holt M, Maher L, Murphy D, Jin F,
et al. Substantial decline in use of HIV preexposure prophylaxis
following introduction of COVID-19 physical distancing restrictions
in Australia: results from a prospective observational study of
gay and bisexual men. J Acquir Immune Defic Syndr. (2021)
86:22–30. doi: 10.1097/QAI.0000000000002514
10. Davey DLJ, Bekker LG, Mashele N, Gorbach P, Coates TJ,
Myer L. PrEP retention and prescriptions for pregnant women
during COVID-19 lockdown in South Africa. Lancet HIV. (2020)
7:e735. doi: 10.1016/S2352-3018(20)30226-5
11. Junejo M, Girometti N, McOwan A, Whitlock G. HIV
postexposure prophylaxis during COVID-19. Lancet HIV. (2020)
7:e460. doi: 10.1016/S2352-3018(20)30146-6
12. Reyniers T, Rotsaert A, Thunissen E, Buffel V, Masquillier C, Van Landeghem
E, et al. Reduced sexual contacts with non-steady partners and less PrEP
use among MSM in Belgium during the first weeks of the COVID-19
lockdown: results of an online survey. Sex Transm Infect. (2020) 97:414-
9. doi: 10.1136/sextrans-2020-054756
13. Charre C, Icard V, Pradat P, Brochier C, Lina B, Chidiac C,
et al. Coronavirus disease 2019 attack rate in HIV-infected
patients and in preexposure prophylaxis users. AIDS. (2020)
34:1765–70. doi: 10.1097/QAD.0000000000002639
14. Chow EPF, Hocking JS, Ong JJ, Schmidt T, Buchanan A, Rodriguez E,
et al. Changing the use of HIV pre-exposure prophylaxis among men
who have sex with men during the COVID-19 pandemic in Melbourne,
Australia. Open Forum Infect Dis. (2020) 7:ofaa275. doi: 10.1093/ofid/
ofaa275
Frontiers in Medicine | www.frontiersin.org 9 April 2022 | Volume 9 | Article 738541

Gao et al. PrEP Adherence During the COVID-19 Pandemic
15. Wang H, Zhang Y, Mei Z, Jia Y, Leuba SI, Zhang J, et al. Protocol for
a multicenter, real-world study of HIV pre-exposure prophylaxis among
men who have sex with men in China (CROPrEP). BMC Infect Dis. (2019)
19:721. doi: 10.1186/s12879-019-4355-y
16. Riddell J, Amico KR, Mayer KH. HIV preexposure prophylaxis: a review.
JAMA. (2018) 319:1261–8. doi: 10.1001/jama.2018.1917
17. Stephenson R, Chavanduka T, Rosso M, Sullivan SP, Pitter RA, Hunter AS,
et al. Sex in the time of COVID-19: results of an online survey of gay,
bisexual and other men who have sex with men’s experience of sex and
HIV prevention during the US COVID-19 epidemic. AIDS Behav. (2021)
25:40–8. doi: 10.1007/s10461-020-03024-8
18. Saag MS, Gandhi RT, Hoy JF, Landovitz RJ, Thompson MA, Sax PE, et al.
Antiretroviral drugs for tre atment and prevention of HIV infection in adults:
2020 recommendations of the International Antiviral Society-USA Panel.
JAMA. (2020) 324:1651–69. doi: 10.1001/jama.2020.17025
19. Smith D, Herbst J, Zhang X, Rose C. Condom effectiveness for HIV
prevention by consistency of use among men who have sex with men
in the United States. J Acquir Immune Defic Syndr. (2015) 68:337–
44. doi: 10.1097/QAI.0000000000000461
20. Sanchez TH, Zlotorzynska M, Rai M, Baral SD. Characterizing the impact of
COVID-19 on men who have sex with men across the United States in April
2020. AIDS Behav. (2020) 24:2024–32. doi: 10.1007/s10461-020-02894-2
21. Buchbinder SP, Glidden DV, Liu AY, McMahan V, Guanira JV, Mayer
KH, et al. HIV pre-exposure prophylaxis in men who have sex with
men and transgender women: a secondary analysis of a phase 3
randomised controlled efficacy trial. Lancet Infect Dis. (2014) 14:468–
75. doi: 10.1016/S1473-3099(14)70025-8
22. Pampati S, Emrick K, Siegler A, Jones J. Changes in sexual behavior, PrEP
adherence, and access to sexual health services because of the COVID-19
pandemic among a cohort of PrEP-using MSM in the South. J Acquir Immune
Defic Syndr. (2021) 87:639–43. doi: 10.1097/QAI.0000000000002640
23. Jewell BL, Mudimu E, Stover J, Ten Brink D, Phillips AN, Smith JA, et al.
Potential effects of disruption to HIV programmes in sub-Saharan Africa
caused by COVID-19: results from multiple mathematical models. Lancet
HIV. (2020) 7:e629-40. doi: 1 0.1 01 6 /S2 3 52 -3 01 8 (20 )302 1 1- 3
24. Anderson L, Caniza M. COVID-19 and preventative medicine for HIV
infected children. Clin Infect Dis. (2020) 73:e2834-5. doi: 10.1093/cid/ciaa1626
25. Rocheleau G, Brumme CJ, Shoveller J, Lima VD, Harrigan PR. Longitudinal
trends of HIV drug resistance in a large Canadian cohort, 1996-2016. Clin
Microbiol Infect. (2018) 24:185–91. doi: 1 0.1 01 6/ j.cmi.2017 .06 .01 4
26. McClung RP, Oster AM, Ocfemia MCB. Transmitted drug resistance among
HIV-1 diagnoses in the United States, 2014-2018. Clin Infect Dis. (2021)
74:1055-62. doi: 10.1093/cid/ciab583
27. Middleton M, Somerset S, Evans C, Blake H. Test@Work texts: mobile phone
messaging to increase awareness of HIV and HIV testing in UK construction
employees during the COVID-19 pandemic. Int J Environ Res Public Health.
(2020) 17:7819. doi: 10.3390/ijerph17217819
28. Amstutz A, Kopo M, Lejone TI, Khesa L, Kao M, Muhairwe J, et al. “If
it is left, it becomes easy for me to get tested”: use of oral self-tests and
community health workers to maximize the potential of home-based HIV
testing among adolescents in Lesotho. J Int AIDS Soc. (2020) 23(Suppl
5):e25127. doi: 10.1002/jia2.25563
29. Haberer JE, Baeten JM, Campbell J, Wangisi J, Katabira E, Ronald
A, et al. Adherence to antiretroviral prophylaxis for HIV prevention:
a substudy cohort within a clinical trial of serodiscordant couples in
East Africa. PLoS Med. (2013) 10:e1001511. doi: 10.1371/journal.pmed.
1001511
30. Luo D, Yan X, Xu R, Zhang J, Shi X, Ma J, et al. Chinese trends
in adolescent marriage and fertility between 1990 and 2015: a
systematic synthesis of national and sub national population data.
Lancet Glob Health. (2020) 8;e954-64. doi: 10.1016/S2214-109X(20)
30130-3
31. Schwartz SR, Nowak RG, Orazulike I, Keshinro B, Ake J, Kennedy
S, et al. The immediate effect of the Same-Sex Marriage Prohibition
Act on stigma, discrimination, and engagement on HIV prevention and
treatment services in men who have sex with men in Nigeria: analysis
of prospective data from the TRUST cohort. Lancet HIV. (2015) 2:e299-
306. doi: 10.1016/S2352-3018(15)00078-8
32. Campion EW, Morrissey S, Drazen JM. In support of same-
sex marriage. N Engl J Med. (2015) 372:1852–3. doi: 10.1056/
NEJMe1505179
Conflict of Interest: Gilead sciences inc. donated all the PrEP drugs for the
CROPrEP.
The authors declare that the research was conducted in the absence of any
commercial or financial relationships that could be construed as a potential
conflict of interest.
Publisher’s Note: All claims expressed in this article are solely those of the authors
and do not necessarily represent those of their affiliated organizations, or those of
the publisher, the editors and the reviewers. Any product that may be evaluated in
this article, or claim that may be made by its manufacturer, is not guaranteed or
endorsed by the publisher.
Copyright © 2022 Gao, Hu, Leuba, Jia, Wang, Huang, Chen, Wang, Zhang, Chu,
Zhang, Wang, Shang, Xu and CROPrEP Study Team. This is an open-access article
distributed under the terms of the Creative Commons Attribution License (CC BY).
The use, distribution or reproduction in other forums is permitted, provided the
original author(s) and the copyright owner(s) are credited and that the original
publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these
terms.
Frontiers in Medicine | www.frontiersin.org 10 April 2022 | Volume 9 | Article 738541
