Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 1
ISSUE BRIEF
Older Immigrants and Medicare
ISSUE BRIEF • APRIL 2019
Georgia Burke, Directing Attorney, Justice in Aging
Natalie Kean, Senior Staff Attorney, Justice in Aging
Table of Contents
Introduction .................................................... 1
Program Eligibility, Enrollment and Costs ...... 1
Paying for Coverage ....................................... 5
Summary of Eligibility and Premium
Assistance Options-LPR and TPS ................... 9
Post Enrollment Issues ................................... 9
Language Access and Medicare .................... 10
Conclusion ...................................................... 11
Endnotes ........................................................ 12
INTRODUCTION
Enrolling in the Medicare program and accessing
its benets can be complex and is often confusing for
older adults. e process can be even more challenging
for older immigrants, some of whom do not have a
signicant work history in the United States, are not
citizens, or have limited English prociency. Almost 7
million U.S. residents age 65 and older are immigrants,
and 4 million Medicare beneciaries are limited English
procient.
1
To assist advocates working with older immigrants
who may qualify for Medicare, this issue brief discusses
Medicare policies and practices most relevant to older
immigrants. Specically, it looks at:
• Eligibility and enrollment, with particular
attention to rules aecting non-citizens
• Help paying for coverage
• Post-enrollment issues potentially aecting
immigrant beneciaries
• Language access rights and resources in Medicare.
e issue brief includes numerous hypothetical
examples. e names and details are created to illustrate
the rules and are not actual case reports.
PROGRAM ELIGIBILITY,
ENROLLMENT AND COSTS
e Social Security Administration (SSA) determines
eligibility and handles enrollment for the two core
Medicare benets: Part A, generally referred to as the
hospital benet, and Part B, which covers physicians
and most other health services. Beneciaries with either
Part A or Part B coverage can enroll in Part D, the
prescription drug benet. e Centers for Medicare and
Medicaid Services (CMS) handles enrollment in Part
D, the prescription drug benet. Beneciaries with both
Part A and Part B coverage have the option to receive
their benets through managed care, called Medicare
Advantage. CMS is in charge of Medicare Advantage
enrollment.
2
Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 2
Premium costs for Medicare
Many older immigrants who immigrated later in life have little or no work history in the United States, a fact
that aects their Medicare costs, and, in some cases, their eligibility.
Part A premiums can be a particular challenge for some immigrants. Most Medicare beneciaries qualify
for Part A coverage without paying a premium. ey qualify based on their work credits (generally 40 quarters,
approximately ten years) or on the work credits of their spouse.
3
ose without the required credits must pay high
premiums for Part A coverage, up to $437/mo. in 2019.
4
Note that work credit requirements are dierent for people
qualifying for Medicare on the basis of disability and that there also are unique rules for people with ESRD.
In addition, Medicare Part B requires a premium payment, which for 2019 is $135.50/mo.
5
Both Part A and
Part B have late enrollment penalties that may apply to individuals who do not enroll when rst eligible.
6
Medicare
Prescription Drug Plans (PDPs) also have premiums that vary depending on the plan, as well as late enrollment
penalties for delays in enrollment.
To purchase Part A, an individual must also enroll in Part B. In contrast, it is possible to enroll only in Part B
and forgo Part A coverage. Individuals can enroll in the Part D prescription drug benet if they have either Part A or
Part B coverage.
Immigration status and enrollment
To enroll in either Part A or Part B, an individual must either be a U.S. citizen or be lawfully present in the
United States. In most cases, as discussed in detail below, a non-citizen who does not qualify for premium-free Part
A must be a lawful permanent resident (LPR) with ve years of continuous residence in the U.S. immediately prior
to Medicare enrollment.
Individuals who are not lawfully present (undocumented) are ineligible to receive any Medicare coverage under
any circumstances.
7
A. Citizens have no length of residency requirements
U.S. citizens face no length of residency requirement to enroll in Medicare, whether or not they have the work
credits to qualify for premium-free Part A.
8
ose who are living abroad and return to the U.S. after they reach
the age of 65, however, can face additional costs and gaps in enrollment if they do not enroll during the Initial
Enrollment Period (IEP) around their 65th birthday. In most cases, they do not have a Special Enrollment Period
(SEP) when they return so must wait until the General Enrollment Period (GEP), which extends from January 1
to March 31 each year, with coverage starting July 1. ey also face late enrollment penalties if they do not enroll
during their IEP, even though, when they are living abroad, they have no access to any Medicare benets.
Case Examples: Citizens living abroad
Mr. Santos, born in the Philippines, came to the United States twenty years ago. He worked and contributed to
Social Security and Medicare since shortly after he arrived. He has been a U.S. citizen for ten years but has lived in
the Philippines for the last four years caring for relatives, who are now deceased. He returned to the United States
in the fall last year, shortly after he turned 68. Because he is a U.S. citizen, he was able to begin his Part A Medicare
immediately. The fact that he reestablished U.S. residence only months ago was irrelevant to his eligibility for Part A
or Part B. Though eligible for Part B, he did however face a delay in enrolling. The fact that he was living overseas and
unable to use Medicare benets did not delay his IEP and there is no Special Enrollment Period for returning citizens.
He will only be able to enroll in Part B during the GEP with enrollment effective July 1. Mr. Santos will also owe a late
enrollment penalty for his Part B premium because he did not enroll during his IEP.

Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 3
Ms. Reyes, who will have her 65th birthday in a few months, came to the U.S. in the same year as Mr. Santos. She
also is a citizen and also spent extended periods out of the country to care for family members. She, however, does
not have the work history needed for premium-free Part A, but she wants to enroll and pay the premiums. Because
Ms. Reyes is a citizen, she can enroll in premium Part A during her IEP and in Part B without any length of residency
requirements. The Social Security Administration (SSA) will not look at her time abroad when processing her
enrollment.
B. Lawfully present non-citizens who qualify for Part A without a premium have no length
of residency requirement
Lawfully present individuals
9
with work credits that qualify them for premium-free Part A also do not face any
length of residency requirement.
10
is includes both LPRs and individuals in Temporary Protected Status (TPS)
who have sucient work credits. Because they qualify for premium-free Part A, these individuals can enroll in both
Part A and Part B without any length of residency requirement.
11
Although advocates for older adults report that they usually see only LPRs and TPS holders with the required
work history, it is possible that other categories of lawfully present individuals, such as Compact of Free Association
(COFA) Migrants or asylees, could accrue enough work credits to qualify for Part A without a premium. In many
cases, these would be younger individuals who qualify for disability-based Medicare with fewer years of work credits.
Case Examples: Lawfully present residents (LPR) with sufcient work credits for Part A
Ms. Morales, originally from El Salvador, has lived and worked in the United States for 13 years holding Temporary
Protected Status. Her work history qualies her for premium-free Part A. She can enroll in both Part A and Part B. The
fact that she is not an LPR will not be considered. It is sufcient that she is lawfully present.
Ms. Lopez is an LPR who came to the U.S. three years ago. She married another LPR shortly after arriving. Her
husband, a long-term U.S. resident, has enough credits for premium-free Part A. Ms. Lopez is turning 65. Because she
can rely on her husband’s work history, she can start her Part A and Part B coverage right away, even though she has
not been a U.S. resident for ve years.
Advocacy tip
Terminology can be confusing. For example SSA and CMS use the term “entitled to Part A benets” to describe
someone who qualies for premium-free Part A. Another possible point of confusion it the fact that, although
”Lawful Permanent Resident” (LPR) is the term used in most immigration contexts for green card holders (and also
used in this issue brief), SSA refers to those individuals as Lawfully Admitted Permanent Residents (LAPR).
C. Non-citizens without the work credits to qualify for premium-free Part A face additional
status and length of residency requirements
Many non-citizen immigrants do not have the work credits to qualify for premium-free Part A. To be eligible for
any Medicare benets, these individuals must 1) be lawful permanent residents (LPR, holding a green card) and 2)
have ve years of continuous residence in the United States immediately prior to Medicare enrollment.
12
e Social
Security Administration determines whether an individual has met the ve-year continuous residency requirements.
When does the ve-year period start? e ve-year period of U.S. residency begins the day the individual
arrives in the U.S. with the intention of establishing a home. e period can start before the individual has LPR
status. e ve-year clock can start, for example, with arrival under refugee or aslyee status. It cannot start with
visitor status since visitors are assumed to be retaining their foreign residence.
13
Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 4
What qualies as “continuing residence”? SSA looks at records of entry into the United States compiled by
the Department of Homeland Security.
14
Temporary absences do not aect “continuous” residence as long as the
individual intends to maintain U.S. residence, but if absences are frequent or of long duration, the agency may
inquire in order to determine whether continued U.S. residency was intended. Examples of evidence of intent could
include continuing to pay U.S. income taxes, maintaining a house or apartment with the individual’s furnishings
and belongings, etc. If an absence is over six months, SSA requires a “strong showing” of intent to retain U.S.
residence.
15
If SSA determines that continuous residence has been broken, the new ve-year period begins on the date that the
individual has returned to the United States.
Case Examples: LPRs without work credits
Mr. Rao, an LPR, came to the United States at age 62 to join the family of his son, a U.S. citizen. He has taken on a
little part-time work but mostly helps care for his grandchildren. Because he does not have enough work history in
the U.S. to qualify for premium-free Part A, Mr. Rao must wait for ve years from his date of entry to the U.S. to qualify
for any Medicare coverage. When he qualies he can enroll in premium Medicare Part A and Part B, or can decide to
enroll only in Part B.
Mr. Lee just turned 65. He has been an LPR since his arrival in the United States eight years ago but does not
have sufcient work history to qualify for Part A without a premium. Most years, he takes a trip back to Korea to visit
family, usually for about six weeks. Mr. Lee applied for Part B Medicare coverage. The Social Security Administration
accepted his application because he is an LPR and, despite several short absences, has met the continuous residency
requirements.
If an LPR subject to the ve-year continuous residency requirement marries someone with premium-free Part A
entitlement, the LPR, after a year of marriage, will also have Part A entitlement based on the spouse’s work history.
e continuous residency requirement will no longer apply.
16
Case Example: LPRs with work credits by marriage
Mr. Williams, a 65 year old LPR, came to the United States from Jamaica last year when he was 64. Because he is
subject to the ve-year continuous residency period, he cannot enroll in Medicare until he is 69. However, next month
he plans to marry Ms. Allen, also an LPR. She has been in the U.S. over 15 years and, because of her work history,
qualies for Part A without premiums. Once they are married for a year, Mr. Williams will be entitled to Part A without
premiums based on Ms. Allen’s record. He won’t have to wait for ve years to pass.
What about Medicare Part D and Part C (Medicare Advantage)? Part D and Part C do not have separate
citizenship or length of residency requirements. Plans are prohibited from requesting from a member any
documentation of citizenship or alien status. CMS provides the ocial status to the plan. If CMS records show that
a plan member is not lawfully present, the plan is required to disenroll the member.
17
Individuals with either Part
A or Part B can join a Part D plan. To join a Medicare Advantage plan under Part C, a beneciary must have both
Medicare Part A and Part B.
Advocacy tip
Enrollment denials or disenrollments arising from errors in SSA and/or CMS records will need to be corrected
with those agencies. ese denials are not subject to Medicare plan appeal processes.

Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 5
PAYING FOR COVERAGE
Even when an immigrant qualies for Medicare coverage, aording that coverage can be a challenge. is is
particularly true for immigrants who must pay premiums to enroll in the Part A benet. e steep Part A premiums
are simply out of reach for many. Premiums for Part B and Part D coverage also add to the nancial burden for
low-income immigrants.
State Medicaid programs can assist with Medicare premiums
ere are several ways that state Medicaid programs can assist low-income immigrants with Medicare costs.
Every state’s standard Aged and Disabled (A&D) Medicaid benet includes payment of the Part B premium for
Medicare beneciaries. e income and asset limits for A&D Medicaid, though they vary by state, are low.
Medicare Savings Programs (MSPs) operated by state Medicaid agencies also oer premium relief and generally
have higher income and asset limits. MSPs do not provide full Medicaid coverage; instead they are specically
designed to assist with Medicare aordability. Federal law sets minimum countable income and asset limits for
MSPs that are higher than for A&D Medicaid, and states have the option to be more generous than federal law
requires. e National Council on Aging (NCOA) has created a chart showing each state’s requirements.
18
e MSP with the richest program benets, the Qualied Medicare Beneciary (QMB) program, can be
particularly helpful to low-income immigrants who must pay a premium for Part A. Under the QMB program, the
state Medicaid agency pays both Part A and Part B premiums. In most states, income must be at or below 100%
of the federal poverty level (FPL) and countable resources may not exceed (for 2019) $7,730 for an individual and
$11,600 for a couple. As the NCOA chart shows, some states have raised income and/or asset cut-os signicantly
and a few have abolished the asset test altogether.
19
In addition to paying Medicare premiums, QMB enrollment protects beneciaries from paying Medicare
deductibles and co-insurance. Note that many QMBs also qualify for A&D Medicaid and are referred to as QMB-
plus.
Two other MSP programs, the Specied Low-income Medicare Beneciary (SLMB) program and the Qualied
Individual (QI) program, only pay Part B premiums. e federal minimum income requirements for these programs
are 135% of FPL and 150%, respectively. Minimum asset requirements for both programs are the same as for the
QMB benet.
State Medicaid programs, including MSPs, have immigration status and length of residency requirements.
20
For
A&D Medicaid and MSPs, individuals must be “qualied” (a status that includes LPR but not TPS). Most qualied
immigrants, including LPRs, are subject to a ve-year bar before qualifying for Medicaid benets. ese restrictions
mean that a Medicare-eligible individual with TPS cannot get help from Medicaid with Part B premiums or
co-insurance. e ve-year bar can also aect Medicaid eligibility for some LPRs.
Advocacy tip
Advocates report that many immigrant families are reluctant to apply for any needed Medicaid benet for older
family members because of fears of estate recovery. It is important to inform beneciaries and their families that the
QMB benet and other MSPs are exempt from estate recovery.

Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 6
Case Examples: Medicare Savings Programs
Ms. Morales, a TPS holder, has Medicare Part A coverage because of her long work history in the U.S. Her income
is below 100% of FPL but she cannot qualify for QMB assistance with her Part B premiums because she is not in
“qualied” status.
Ms. Gonzales, an LPR, gets Part A without paying a premium based on her husband’s work history. Her income and
assets qualify her for the SLMB benet but she only has three years of continuous residence in the U.S. She will have
to wait another two years before she can enroll in SLMB to get help with her Part B premiums.
Enrolling in the QMB program can be challenging
As discussed above, the QMB benet can be particularly helpful to low-income immigrants who must pay a
premium for Part A. e mechanics and timing of enrolling in the QMB program, however, can be complex.
Enrollment procedures depend on the state and on whether the individual already is enrolled in Part B. For those
who are not enrolled in Part B and/or who are in “group payer states” as discussed below, enrollment may require
visits to both the Social Security oce to apply for “conditional” Part A enrollment, and to the state Medicaid
agency to apply for QMB enrollment.
In the majority of states (identied as “Part A buy-in states”), individuals can apply for QMB coverage at any time
of the year and coverage begins in the month immediately following approval. In 14 states (identied as “group payer
states”), however, people without premium-free Part A may only apply at SSA for conditional Part A enrollment
during the General Enrollment Period (January 1-March 31) each year,
21
with QMB enrollment beginning no
earlier than July 1.
A Justice in Aging fact sheet
22
and recently-issued clarifying guidance from SSA detail the specic steps needed to
apply in each set of states.
23
Advocacy tip
Advocates should give their clients step-by-step guidance so that they follow through with all needed procedures.
Particularly in group payer states, calendared reminders and follow-up may be needed to ensure that clients
successfully navigate the enrollment process.
Case Example: Enrolling in QMB
Mrs. Chen is 66 and lives in Arizona, a group payer state. She came to the U.S. seven years ago and has met the
status and residency requirements to qualify for Medicare. Since she has no work history, she has not enrolled in
Medicare because she cannot pay the premiums, especially the Part A premium, which tops $440/mo. In June, she
meets with an advocate who tells Mrs. Chen that, with her income and assets, she qualies for the QMB program,
which will pay both her Part A and Part B premiums. She tells Mrs. Chen, however, that she must wait until January to
go to SSA and apply for conditional Part A enrollment and for Part B. With Mrs. Chen’s consent, the advocate also
tells her daughter and urges both of them to put the date on their calendars. In December, the advocate contacts
both Mrs. Chen and her daughter to remind them to make an appointment with SSA in January and, after applying for
conditional enrollment at SSA, to go directly to the state Medicaid ofce to apply for QMB. The advocate follows up
in late January to make sure that Mrs. Chen took the required steps. She did, and nally on July 1, to her great relief,
Mrs. Chen gets both Part A and Part B coverage without premiums. Mrs. Chen, because of her QMB status, is also
protected from payment of co-insurance and deductibles.Her QMB enrollment also automatically qualies her for the
Part D Low-income Subsidy (discussed below) to help her with prescription drug co-insurance.

Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 7
Marketplace enrollment offers an alternate coverage option
Immigrants who do not qualify for premium-free Part A can also consider enrolling in a Qualied Health Plan
(QHP) in the Marketplace and applying for nancial assistance in the form of premium tax credits and cost-sharing
reductions.
QHPs are available to LPRs as well as individuals on non-immigrant visas and with other status, including many
temporary status categories.
24
Immigrants who are eligible to enroll in QHPs and do not have other “minimum
essential coverage” may also qualify for premium tax credits and cost-sharing reductions to help them aord
coverage.
25
ere are no length of residency requirements for QHPs or for premium tax credits and cost-sharing
reductions. Further, lawfully present individuals, unlike citizens, can receive premium tax credits and cost
sharing reductions, even if their income is below 100% of FPL if they are ineligible for Medicaid because of their
immigration status.
26
When sorting through beneciary eligibility and enrollment options, it is important to remember that, though
there are signicant variations among the states, QMB income counting rules are grounded on SSI income counting
rules. In contrast, Marketplace rules on premium tax credits and cost-sharing reductions apply Modied Adjusted
Gross Income (MAGI) rules.
27
Depending on an individual’s income and circumstances, getting coverage through the Marketplace may be less
expensive than paying for Part A. ose who choose Marketplace coverage rather than Medicare need to be aware
that, if they later decide to switch to Medicare, they can face late enrollment penalties for both Part A and Part B.
28
ey also may face gaps in coverage because they may only be able to enroll in Medicare during the annual General
Enrollment Period.
29
Because of the range of visa and status categories for which Marketplace enrollment is permitted and because
there is no length of residency requirement, the Marketplace also is an option for older adults who do not currently
qualify for Medicare at all, including LPRs who are still in their ve-year waiting period.
Advocacy tip
Advocates should remind clients choosing Marketplace coverage that, even if their income is below tax ling
requirements, they need to le income tax returns in order to get MAGI-based subsidies.
Case Examples: Marketplace and Medicare
Ms. Park is an LPR who is eligible for Medicare but does not qualify for premium-free Part A. Her income is at 200%
FPL, which is too high to qualify for the QMB program in her state. Because her income is low enough to qualify her
for premium tax credits and cost-sharing reductions in the Marketplace, she decides to enroll in a Qualied Health
Plan. She will face both Part A and Part B enrollment penalties if she later decides to enroll in Medicare and will only
be able to do so during certain times of year.
Mr. Jones is an LPR who arrived in the U. S. when he was 62. He is now 66 and enrolled in a Marketplace plan with
premium tax credits and cost-sharing reductions. Next year he will have been in the U.S. for ve years. At that time he
will become eligible for Medicare and, because of his low income, he will also qualify for his state’s Medicaid program.
He will lose his eligibility for Marketplace subsidies so he will switch from the Marketplace to Medicare. His Medicaid
coverage will assist with his Medicare costs.

Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 8
Some people choose to enroll only in Part B
Enrolling only in Medicare Part B and not in Part A is an available option for people who face steep Part A
premiums but don’t qualify for either subsidies for Marketplace coverage or QMB assistance for Medicare premiums.
Part B enrollment allows them to also enroll in Part D and, if they qualify, to get the Low-Income Subsidy (LIS) to
help pay for Part D costs (see below). is course is far from ideal because it leaves an individual without coverage
for hospital costs. However, it is an available option. If these individuals later decide to enroll in Part A, they can face
late enrollment penalties and also may be limited to enrolling during the General Enrollment Period with coverage
not starting until July. If they enroll in Part B and not in Part D, they could also face Part D late enrollment
penalties.
Case Example: Declining Part A coverage
Mr. Singh came to the U.S. eight years ago. He is now 65, LPR and eligible for Medicare but not for premium-free
Part A. From his career in India, he has a pension and a small nest egg, disqualifying him for Medicaid or Marketplace
subsidies. Because has always been healthy, he decides to conserve resources and only enroll in Part B and not in
Part A. By doing so, he will have coverage for doctor visits but risks wiping out his nest egg if he needs hospital care.
Though he currently only takes one inexpensive generic drug, he enrolls in a low cost Part D plan so that he will not
face late enrollment penalties if he later nds that his drug coverage needs increase.
The Part D Low Income Subsidy (“Extra Help”) can reduce prescription drug costs
Beneciaries who qualify for Part D, i.e., those who are enrolled in either Part A or Part B, also may be eligible
for the Part D Low Income Subsidy (LIS or “Extra Help”).
30
Because LIS asset and income limits are higher than
those for QMB and other Medicare Savings Programs, some individuals with higher incomes may qualify for this
benet. e Social Security Administration determines LIS eligibility. Individuals may apply with SSA in-person,
on-line or by phone.
ere are no additional immigration status or length of U.S. residency requirements for LIS beyond what is
needed for Part A and Part B eligibility.
31
LIS enrollment is automatic for Medicare beneciaries receiving SSI and
for those enrolled in any Medicaid program, including Medicare Savings Programs such as the QMB program.
Others can apply by contacting the Social Security Administration and meeting income and asset eligibility
requirements.
32
Instructions for applying are available in 18 languages.
33
Case Example: Extra Help v. QMB
Ms. Morales, a low-income TPS holder with premium-free Part A, successfully applied for the Part D Low Income
Subsidy. Although she had been unable to enroll in the QMB program because she was not a “qualied” immigrant,
that was not a factor in evaluation her LIS application. Having LIS gives her with signicant relief from prescription
drug costs.
Policy Watch
In 2018, the Department of Homeland Security proposed new regulations that would treat receipt of the
LIS benet as a factor in determining whether an applicant for LPR status would likely be a public charge.
34
As
proposed, the changes would be prospective and not aect current LIS enrollees. Advocates will want to monitor the
progress of this proposal.
35

Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 9
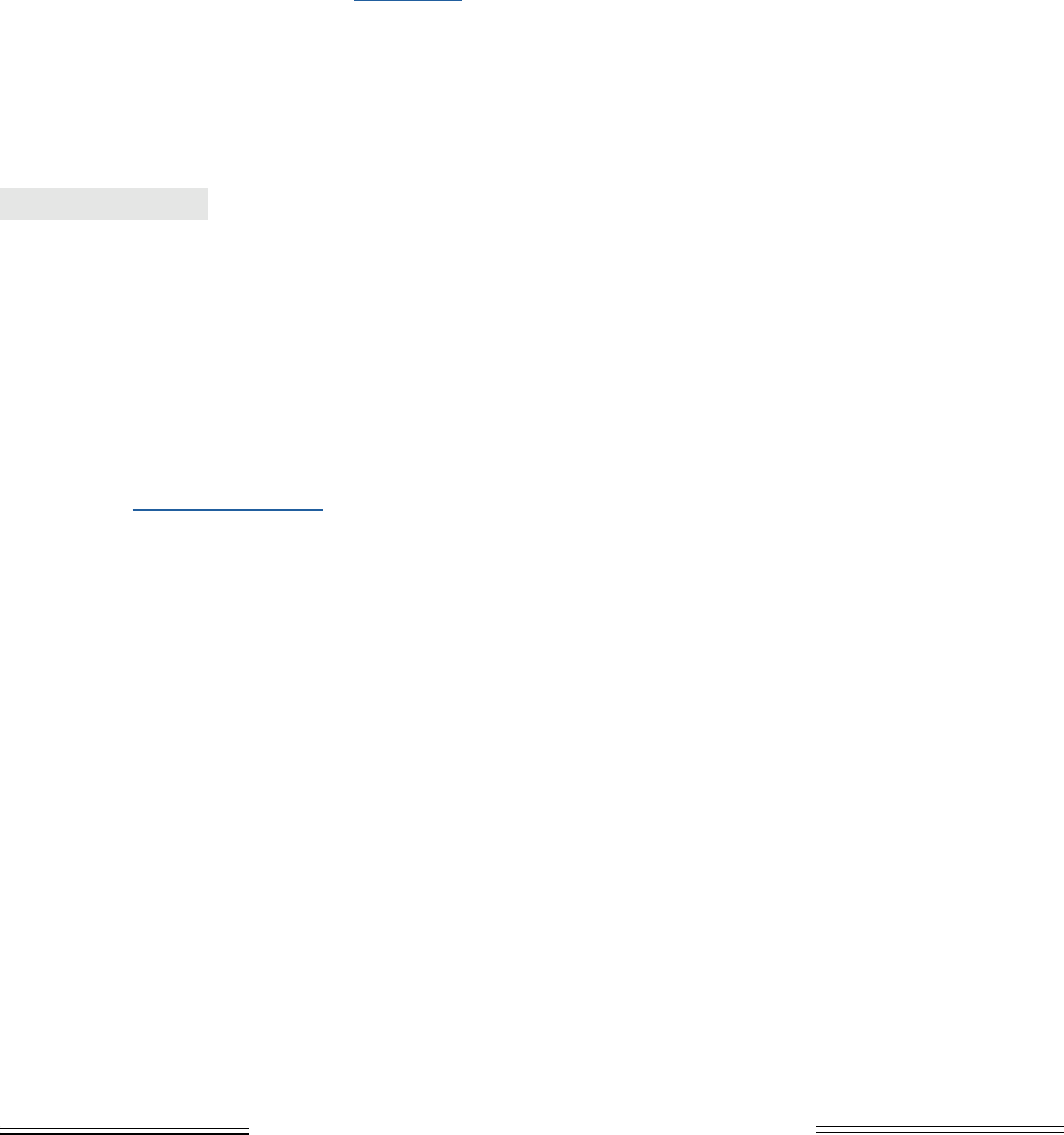
SUMMARY OF ELIGIBILITY AND PREMIUM ASSISTANCE
OPTIONS—LPR AND TPS
MEDICARE
ELIGIBILITY
AVAILABLE PROGRAMS TO HELP W/ COSTS
Does 5 yr.
residence apply?
Medicaid and MSPs Part D LIS
Are Marketplace
subsidies available?
LPR—qualifying
work record
No
Yes w/ 5 yr
residence
Yes No
LPR –w/out
qualifying work
record
Yes but w/ Part A
premium
Yes w/ 5 yr.
residence
Yes if enroll in
either A or B
Yes*
TPS—qualifying
work record
No No Yes No
TPS-w/out
qualifying work
record
No N/A N/A
Yes
*For those with income below 100% FPL, subsidies are available only if they cannot qualify for Medicaid because of
their immigration status.
POST ENROLLMENT ISSUES
Medicare does not pay for services outside the U.S.
Many immigrants, particularly those who are citizens, may spend signicant time overseas during their
retirement. Medicare does not cover health care provided outside the United States.
36
Medicare premium payment liabilities continue even when a beneciary is abroad.
e obligation to continue payment of Medicare premiums continues when a beneciary spends time abroad. If a
beneciary stops paying Part A or Part B premiums, late enrollment penalties can arise and the beneciary may have
to wait until the next Medicare General Enrollment Period to reapply, resulting in many months without coverage.
Beneciaries who have Medicare coverage and spend time abroad should be careful about how they handle their
Medicare premiums.
Case Example: Time abroad
Ms. Adebayo, originally from Nigeria, is a U.S. citizen with Medicare Part A and Part B coverage. She rushed back
to Nigeria after a niece died suddenly, leaving several small children. She now realizes that she is needed for an
indenite time to make sure that the children are properly cared for. Though she has the option of stopping her Part B
premiums, she decides that she will let SSA continue to deduct the premium from her monthly Social Security benet.
She does not want to face late enrollment penalties when she returns or have a gap in coverage while she waits for an
enrollment period to re-enroll.

Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 10
LANGUAGE ACCESS AND MEDICARE
Older immigrants with limited English prociency need language assistance to understand their benets, address
their health care needs, and exercise their rights under Medicare.
Governing statutes
e statutory bases for language access rights in Medicare are found in Title VI of the Civil Rights Act of 1964
37
and the Health Care Rights Law, Section 1557 of the Aordable Care Act.
38
Section 1557 applies the provisions
of Title VI to the Department of Health and Human Services (HHS) and to health programs and activities, any
part of which receive Federal nancial assistance from HHS. e HHS Oce for Civil Rights has enforcement
responsibility. In addition, Section 1557 provides for a private right of action.
39
HHS takes the position that those physicians and other providers who participate in Medicare only as Part B
providers and do not receive any other Federal nancial assistance from HHS are not subject to Section 1557, but
asserts that almost all physicians in fact are covered because they accept Federal nancial assistance from sources
other than Medicare Part B.
40
Regulations and guidance
e HHS Oce for Civil Rights and CMS have each adopted regulations implementing these statutes. CMS has
also developed sub-regulatory guidance for Medicare Advantage plans and Prescription Drug Plans. CMS has noted,
however, that plan and provider obligations under the statutes may be broader than the specic requirements in its
guidance and advises plans to independently assess their obligations under these statutes.
HHS regulations require free, accurate, and timely language assistance when needed to provide meaningful
access to individuals with limited English prociency.
41
e HHS regulations do not identify specic instances
where interpreter services are required or specic documents that must be translated, but, in commentary, the
agency provides guidance on factors to be considered in enforcement.
42
Interpreter and translation services must be
provided by “qualied” interpreters and translators.
43
Covered entities may not require that individuals provide their
own interpreters and may not use a minor child except in cases of emergency.
44
Medicare plans also are required to
include taglines with “signicant” documents and communications. e tagline must provide information in the top
15 languages of the state announcing the availability of language services.
45
Medicare regulations governing health and prescription drug plans include additional specic requirements.
ey require that Medicare Advantage and Medicare Prescription Drug Plans must translate “vital materials” into
any non-English language that is the primary language of at least ve percent of the individuals in a plan benet
package service area.
46
In the Medicare Communications and Marketing Guidance (MCMG), CMS identies vital
documents as including most basic marketing materials (application, evidence of coverage and summary of benets,
provider and drug lists, etc.); enrollment and disenrollment communications; and appeals and grievance notices.
47
Except for a few Medicare Advantage plan service areas, the ve percent threshold means that Spanish is the only
language required.
Advocacy Tip
If clients are in Medicare Advantage plans are having problems getting needed interpreter services, the most
expeditious route to getting individual issues addressed is likely to be ling a grievance with the plan and/or a
complaint with CMS at 1-800-Medicare.
Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 11
MCMG also requires plan call centers to have interpreter services in all languages.
48
Wait times should not be
excessive.
Agency resources
e Medicare consumer website, Medicare.gov, is available in Spanish.
49
e Medicare & You Handbook is
also published in Spanish. An “Information in Other Languages” page
50
lists all non-English language forms and
publications available from CMS. e 1-800-Medicare help line provides free interpretation services in all languages
and, as noted above, all call centers for Medicare Part D plans and Medicare Advantage plans are required to do so
as well.
51
e Marketplace website, HealthCare.gov, also is available in Spanish. HealthCare.gov has non-English resources
as well.
52
e Marketplace Call Center and QHPs are also required to provide interpretation services.
53
Advocacy Tip
CMS data show that very few individuals who speak languages other than Spanish ask for interpreter services
when calling 1-800-Medicare. Plan level data are not available, but it appears that uptake there as well is limited.
is suggests that LEP individuals are either unaware of the free service or reluctant to ask for it. Advocates should
explain the availability of these services to their clients and encourage their use when they have questions or if they
receive a document from Medicare or from their MA plan in English that they do not understand.
CONCLUSION
Advocates can assist their older immigrant clients to navigate Medicare enrollment, costs, and language hurdles.
Justice in Aging is available to work with advocates as they encounter Medicare issues for their immigrant clients.
Contact info@justiceinaging.org.
We would like to acknowledge and thank Nancy Lorenz of Greater Boston Legal Services and Vicky Pulos of
Massachusetts Law Reform Institute for their valuable contributions to this report.
Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 12
ENDNOTES
1 Migration Policy Institute, “State Immigration Data Proles, United States,” available at www.migrationpolicy.org/data/state-pro-
les/state/demographics/US; CMS Oce of Minority Health, “Understanding Communication and Language Needs of Medicare
Beneciaries,” 8, 10 (Apr 2017), available at www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/Issue-Briefs-Under-
standing-Communication-and-Language-Needs-of-Medicare-Beneciaries.pdf.
2 For a description of the parts of Medicare and services covered, see CMS “Medicare & You” (2019), available at www.medicare.gov/
forms-help-resources/medicare-you-handbook/download-medicare-you-in-dierent-formats.
3 42 C.F.R. § 406.10. See also 42 C.F.R. § 406.12 which applies to individuals who qualify for premium-free Part A based on
disability determination by the Social Security Administration, and 42 C.F.R. § 406.13, which applies to individuals with ESRD.
See CMS, “Original Medicare (Part A and B) Eligibility and Enrollment,” available at www.cms.gov/Medicare/Eligibility-and-En-
rollment/OrigMedicarePartABEligEnrol/. e POMS provisions concerning Part A entitlement are found at subchapter HI 00801,
available at https://secure.ssa.gov/apps10/poms.nsf/subchapterlist!openview&restricttocategory=06008.
4 SSA requires fewer work credits for individuals under 65 who qualify for Medicare on the basis of disability, using a formula based
on the applicant’s age when becoming disabled. For a chart of credits needed based on age, see SSA, “How You Earn Credits” (2019),
p. 3, available at www.ssa.gov/pubs/EN-05-10072.pdf.
5 CMS, “Medicare costs at a glance,” available at www.medicare.gov/your-medicare-costs/medicare-costs-at-a-glance.
6 For a summary of late enrollment penalties, see www.mymedicarematters.org/enrollment/penalties-and-risks/. To calculate late
enrollment penalties see www.medicareinteractive.org/get-answers/medicare-health-coverage-options/original-medicare-enrollment/
medicare-part-b-late-enrollment-penalties.
7 e SSA POMS GN 00303.800 has created some confusion about whether this prohibition applies to undocumented persons with
ESRD. e POMS provision notes that there are no residency, citizenship or alien status requirements for Medicare entitlement
based on ESRD. Entitlement, however, must be distinguished from actually access to the benet. Pursuant to the Personal Respon-
sibility and Work Opportunity Reconciliation Act of 1996 (PRWORA), no Medicare payments can be made for an undocumented
beneciary. See SSA POMS RS 00204.010(B), available at https://secure.ssa.gov/apps10/poms.nsf/lnx/0300204010. us, as with
other Medicare benets, ESRD-based Medicare is only available to those non-citizens who are lawfully present.
8 42 C.F.R. § 406.20.
9 For the denition of lawfully present for purposes of SSA benets as well as Medicare determinations, see 8 C.F.R. § 1.3 and SSA
POMS RS 00204.00 available at https://secure.ssa.gov/apps10/poms.nsf/lnx/0300204010.
10 42 U.S.C § 1395o; 42 C.F.R. § 406.10 (a)(1).
11 42 U.S.C. § 1395o; 42 C.F.R §§406.10 and 407.10(a)(1).
12 For Part A, these restrictions are found at 42 U.S.C. § 1395i-2(a)(3) and 42 C.F.R. § 406.20. e restrictions for Part B are found at
42 U.S.C. § 1395o(2) and 42 C.F.R § 407.10(a)(2).
13 SSA POMS GN 00303.800(B)(4), available at https://secure.ssa.gov/apps10/poms.nsf/lnx/0200303800.
14 Id.
15 Id. See also SSA POMS GN 00303.740 describing SSA procedures to determine residence, available at https://secure.ssa.gov/apps10/
poms.nsf/lnx/0200303800.
16 SSA POMS GN 00303.800(A)(2), available at https://secure.ssa.gov/apps10/poms.nsf/lnx/0200303800.
17 Medicare Managed Care Manual, Ch. 2, at 50.2.7, available at www.cms.gov/Medicare/Eligibility-and-Enrollment/MedicareMang-
CareEligEnrol/Downloads/CY_2019_MA_Enrollment_and_Disenrollment_Guidance.pdf.
18 See NCOA, Chart: Medicare Savings Programs: Eligibility and Coverage, available at www.ncoa.org/wp-content/uploads/medi-
care-savings-programs-coverage-and-eligibility.pdf.
Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 13
19 Id.
20 See CMS, “Eligibility for Non-Citizens in Medicaid and CHIP” (Nov. 2014), available at www.medicaid.gov/medicaid/out-
reach-and-enrollment/downloads/overview-of-eligibility-for-non-citizens-in-medicaid-and-chip.pdf.
21 ese states, called “Group Payer” states, are: AL, AZ, CA, CO, IL, KS, KY, MO, NE, NJ, NM, SC, UT, and VA.
22 Justice in Aging, “SSA Claries Handling of Medicare Part A Conditional Applications,” available at www.justiceinaging.org/
wp-content/uploads/2018/08/SSA-Claries-Handling-of-Medicare-Part-A-Conditional-Applications.pdf.
23 SSA POMS, HI 00801.140, available at https://secure.ssa.gov/poms.nsf/lnx/0600801140.
24 See “Immigration status and the Marketplace,” available at www.healthcare.gov/immigrants/immigration-status/. For additional de-
tail see NILC, “’Lawfully Present’ Individuals Eligible under the Aordable Care Act,” available at www.nilc.org/issues/health-care/
lawfullypresent/.
25 Ctr. on Budget & Policy Priorities, “Key Facts: Immigrant Eligibility for Health Insurance Aordability Programs,” (2015), available
at www.healthreformbeyondthebasics.org/key-facts-immigrant-eligibility-for-coverage-programs/.
26 26 U.S.C. § 36B(c)(B). See also HealthCare.gov “Coverage for lawfully present immigrants,” available at https://www.healthcare.
gov/immigrants/lawfully-present-immigrants/.
27 For a primer of MAGI counting rules, see Nat’l Health Law Program, “Advocate’s Guide to MAGI,” available at https://healthlaw.
org/resource/advocates-guide-to-magi-updated-guide-for-2018/.
28 If they don’t enroll in either Part A or Part B, they would not face Part D late enrollment penalties. Late enrollment calculations
are only triggered after the individual becomes eligible for Part D. Part D requires either Part A or Part B coverage. See 42 C.F.R. §
423.38 and 423.46.
29 CMS has created a Medicare-Medicaid Master FAQ that discusses the details of interaction between Medicare and Marketplace
coverage, available at www.cms.gov/Medicare/Eligibility-and-Enrollment/Medicare-and-the-Marketplace/Overview1.html. See
especially Questions A.6, A.8 and A.9.
30 See www.ssa.gov/benets/medicare/prescriptionhelp/.
31 HHS has not determined the Low Income Subsidy to be a federal “public benet.”See ASPE, “Summary of Immigrant Eligibility Re-
strictions Under Current Law,” available at https://aspe.hhs.gov/basic-report/summary-immigrant-eligibility-restrictions-under-cur-
rent-law. us eligibility is not limited to “qualied” immigrants.
32 See SSA Extra Help webpage at www.ssa.gov/benets/medicare/prescriptionhelp/ for information on the program and links to ap-
plication forms. For details of eligibility and benet levels, see also a helpful chart from the National Council on Aging, available at
www.ncoa.org/wp-content/uploads/part-d-lis-eligibility-and-benets-chart.pdf.
33 See SSA, “Extra Help Information in Other Languages,” available at www.ssa.gov/benets/medicare/prescriptionhelp/other-languag-
es.html.
34 For an overview of the impact of the public charge proposal on older adults, see Justice in Aging, “Public Charge: A reat to the
Health & Well-being of Older Adults in Immigrant Families,” (Oct. 2018), available at www.justiceinaging.org/wp-content/up-
loads/2018/09/Public-Charge_A-reat-to-the-Health-Wellbeing-of-Older-Adults-in-Immigrant-Families.pdf.
35 Justice in Aging will alert its network to any signicant developments. Another good source of information is the Protecting Immi-
grant Families website, available at https://protectingimmigrantfamilies.org/about-us-2/.
36 ere are minor exceptions for people in transit between the continental U.S. and Alaska and for emergency use of a hospital across
the border that is closer than the nearest U.S. facility.
37 42 U.S.C. § 2000d et seq.
38 42 U.S.C. § 18116.
Justice in Aging •
www.justiceinaging.org
• ISSUE BRIEF • 14
39 45 C.F.R. § 92.301. See also discussion at 81 Fed. Reg. 31376, 31439-40 (May 18, 2016)(hereinafter “Final Rule”), available at www.
govinfo.gov/content/pkg/FR-2016-05-18/pdf/2016-11458.pdf.
40 See discussion at 80 Fed. Reg. 54172, 54195 (Sept. 8, 2015), available at www.govinfo.gov/content/pkg/FR-2015-09-08/pdf/2015-
22043.pdf and Final Rule at 31383, supra note 24.
41 45 C.F.R. § 92.201 (a) and (c).
42 See Final Rule at 31416, supra note 41.
43 e denition of qualied interpreter and qualied translator are found at 45 C.F.R. § 92.4.
44 45 C.F.R. § 92.201(e). See also commentary at Final Rule 31417-18, supra note 41.
45 45 C.F.R. § 92.8. Note however that a joint Report to the President by HHS, the Department of the Treasury and the Department
of Labor recommended scaling back the regulation requiring inserts, asserting that the requirement is costly and wasteful. See “Re-
forming America’s Healthcare System rough Choice and Competition,” p. 75, available at www.hhs.gov/sites/default/les/Reform-
ing-Americas-HealthCommunications and Marketing Guidelines-System-rough-Choice-and-Competition.pdf.
46 42 C.F.R. § 422.2268(a)(7) and 42 C.F.R. § 423.2268(a)(7).
47 e full list of communications subject to translation requirements is found at MCMG at 100.4, available at www.cms.gov/Medi-
care/Health-Plans/ManagedCareMarketing/CY2019_Medicare_Communications_and_Marketing_Guidelines.pdf. at list is
eective as of January 1, 2019.
48 Id. at 30.3.
49 https://es.medicare.gov/.
50 www.medicare.gov/about-us/other-languages/information-in-other-languages.html.
51 MCMG, supra note 49 at 30.3, available at www.cms.gov/Medicare/Health-Plans/ManagedCareMarketing/CY2019_Medicare_
Communications_and_Marketing_Guidelines.pdf.
52 www.healthcare.gov/language-resource/.
53 45 C.F.R. § 155.205(c).
